Background
Corneal neuropathic pain is pain in the eye, face or head with ocular symptoms including stinging, burning, irritation, in the absence of noxious stimuli.¹ Slit lamp examination is typically unremarkable.² Scleral lenses may help mitigate symptoms and disrupt the pain cycle in some patients despite a normal exam.³
Case History
A 68-year-old male was referred for evaluation of corneal neurotrophic pain in the contact lens clinic. He complained of bilateral eye pain, tearing, itching and redness for 3 years.
Ocular history: Neuropathic eye pain, blepharospasm, and cataract extraction in 2022 bilaterally.
Prior treatments included artificial tears, eyelid hygiene, Lipiflow with gland expression, intense pulsed light treatment, topical methylprednisolone, topical intravenous immunoglobulin, autologous serum tears, erythromycin ointment, doxycycline, low dose naltrexone and fluoxetine.
Clinical Findings
| OD | OS | |
Visual acuities (sc) | 20/20 | 20/20 | |
IOP | 12 | 12 | |
External Adnexa | Intermittent, forceful spasm | Intermittent, forceful spasm | |
Lids/Lashes | Inspissated meibomian glands | Inspissated meibomian glands | |
Conjunctiva/Sclera | Conjunctivochalasis | Conjunctivochalasis | |
Cornea | Clear, poor tear film | Clear, poor tear film | |
Anterior Chamber | Deep and quiet | Deep and quiet | |
Iris | Flat, reactive | Flat, reactive | |
Lens | PCIOL | PCIOL | |
Additional Testing | OD | OS | |
Tear Break Up Time | 3 sec | 1 sec | |
MMP-9 | Strong + | Strong + | |
Schirmer’s | 12 | 10 | |
Proparacaine | 4/10 pain pre-and post-proparacaine instillation | ||
In vivo confocal microscopy | Reduced nerve density and beading of nerves | ||
Lab work up | |||
TSH | Negative | ||
ANA | Negative | ||
Sjogren’s Panel | Negative (Salivary Protein IgG, IgA, IgM) | ||
Table 1 – Diagnostic dry eye testing and lab work up
Treatment/Management
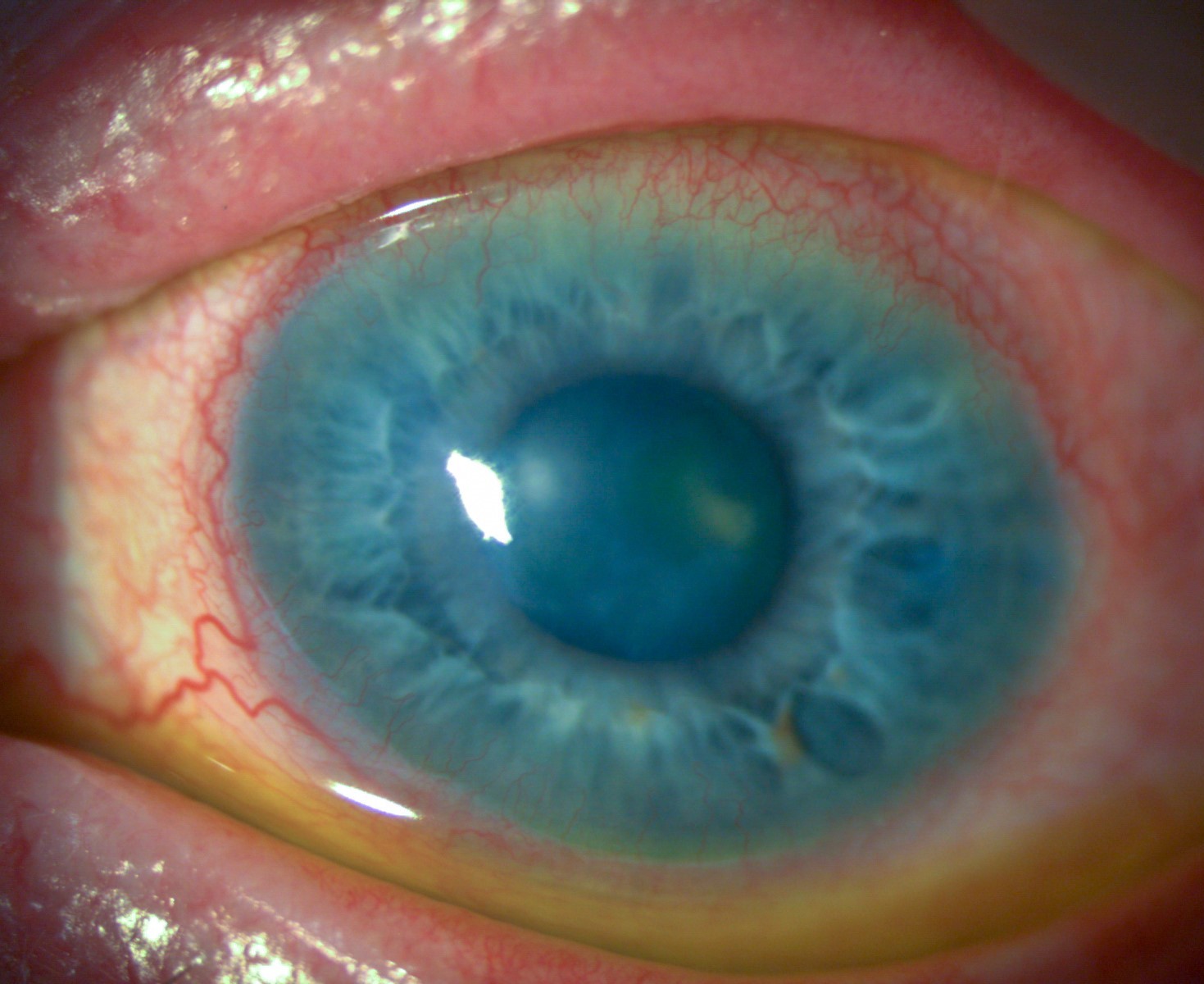
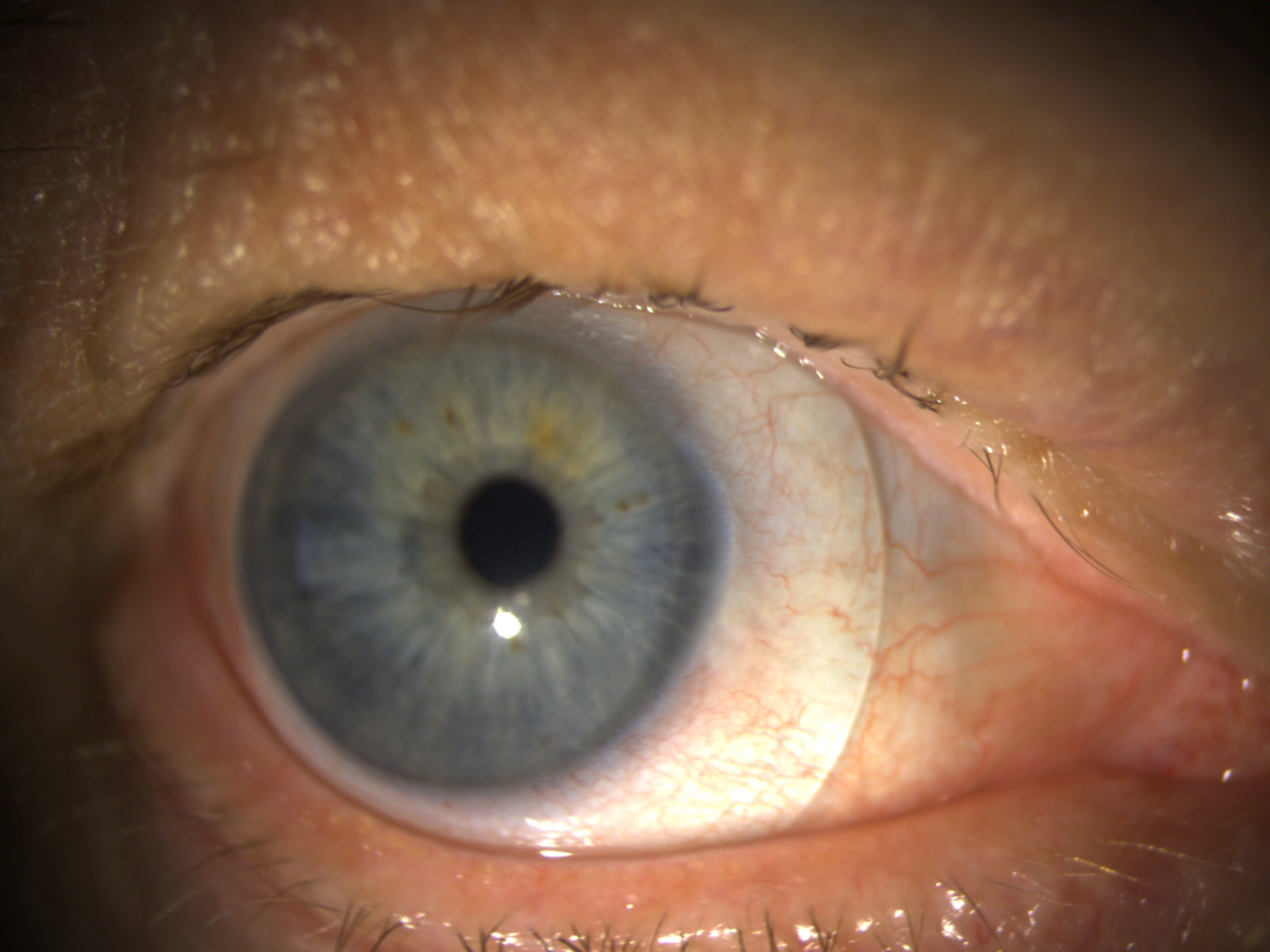
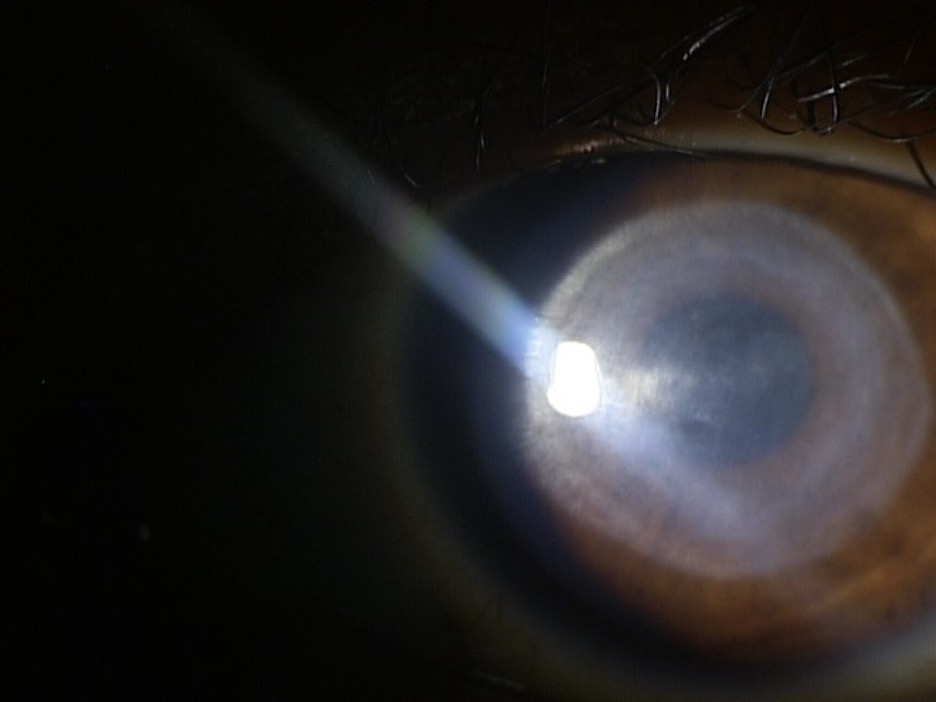
A scleral contact lens was designed for the patient (Table 2, Figure 1-3).
He was also referred to an oculoplastics specialist and treated with 30 units of periorbital botulinum toxin A for blepharospasm (Figure 4).
| Material | Base Curve | Diameter | Rx | Additional Specs |
OD | 7.69 | 17.0 | +0.56 | 3098 FSE0 | |
OS | 8.10 | 17.0 | +3.01 | 2924 FSE0 |
Table 2 – Scleral lens parameters designed using Eaglet Corneoscleral Profilometry
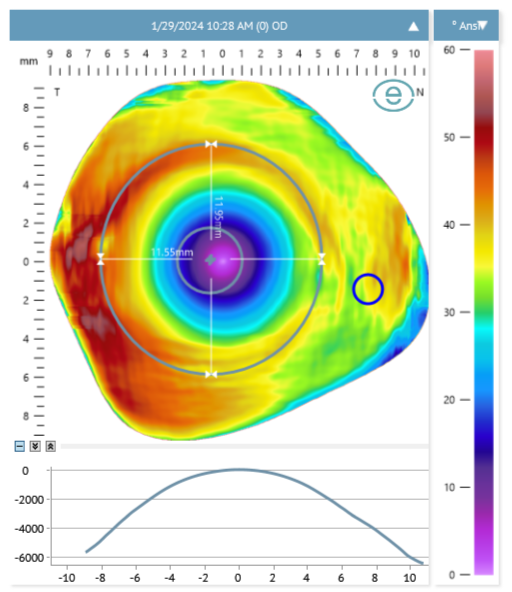
Figure 1: Corneoscleral profilometry mapping of right eye marking nasal pinguecula, HVID and pupil.
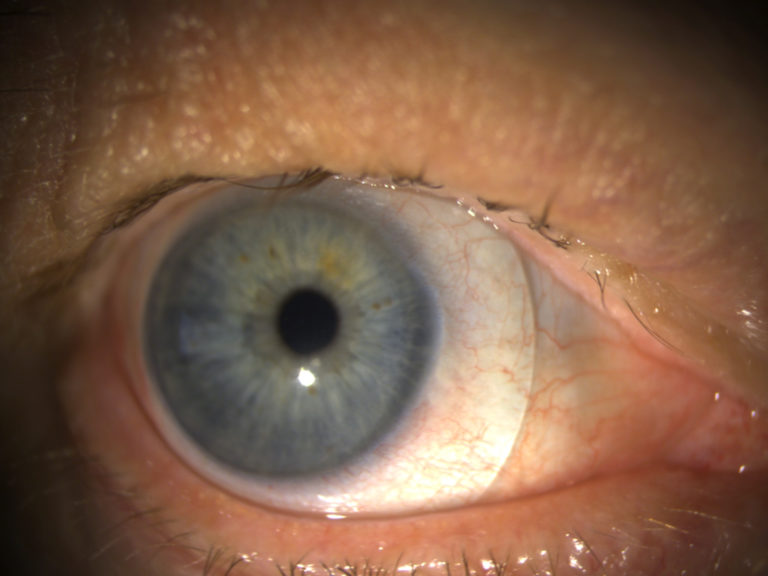
Figure 2: Scleral lens on the right eye.
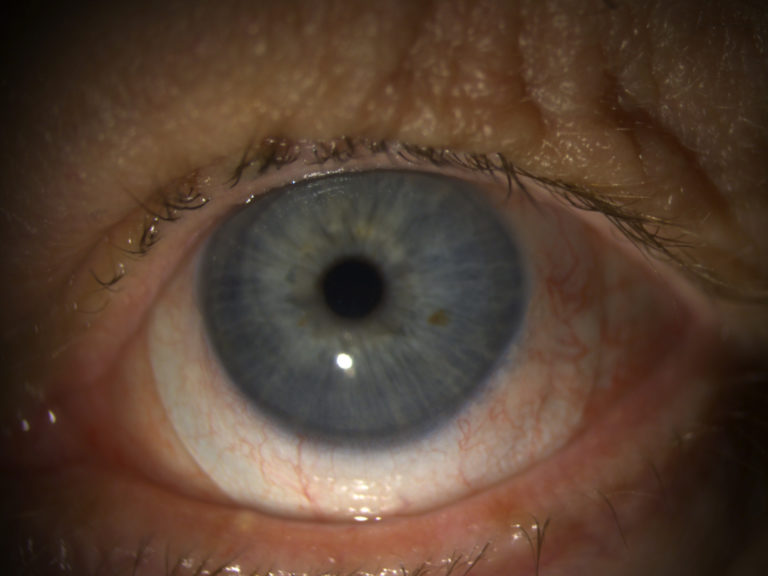
Figure 3: Scleral lens on the left eye.
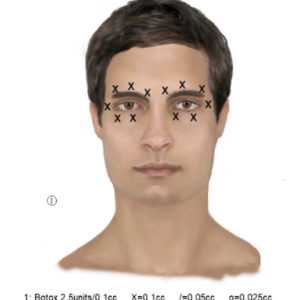
Figure 4: Botox injection to bilateral periocular areas.
Follow Up
The patient returned after scleral lens application and removal training and reported comfortable wear for 12 hours. He denied eye pain or visual blurring during scleral lens wear. He continued preservative-free artificial tears every 2 hours.
After 6 months, he has continued daily scleral lens use with excellent ocular comfort. He follows with his oculoplastics specialist for treatment every 3 months.
Discussion
Diagnosing neuropathic corneal pain involves symptoms assessment, functional somatosensory testing such as the proparacaine challenge test, assessment of nerve density and morphology in vivo confocal microscopy and clinical examination of ocular co-morbidities.²
Our patient had reduced nerve density and beading of nerves in vivo confocal microscopy. In addition, clinical examination of his ocular surface did not correlate with his symptoms and complaints in office. Since there are multiple components involved in development and maintenance of neuropathic corneal pain, there is no single treatment that is effective.
Conclusion
This case highlights the benefits of collaborative care of a patient with neuropathic eye pain utilizing a multidisciplinary approach. This patient benefited from therapeutic scleral lenses as well as blepharospasm management to improve ocular comfort.