Introduction by Martin Conway
In Orthokeratology, the central cornea is flattened by an amount sufficient for the patient to be able to see clearly without lenses. A peripheral ring of power is also created which is approximately equal but opposite to the target refraction i.e. a -3.00 change at the centre of the treatment zone will produce +3.00 at the periphery. This would leave a child fitted with ortho k at the early stages of progression, say -1.00 refraction, with less plus power (+1.00) at the periphery and therefore less of an effect on progression.
Lens designs which produce more plus at the periphery than a conventional design have existed for some time but at the recent EFCLIN meeting in Portugal, Dr Jaume Paune was a keynote speaker and I thought that his presentation “An OK lens is not a Myopia Control Lens” contained findings from his recent studies to warrant inclusion in Global Insight. Jaume has summarised his presentation below and the full study may be accessed here.
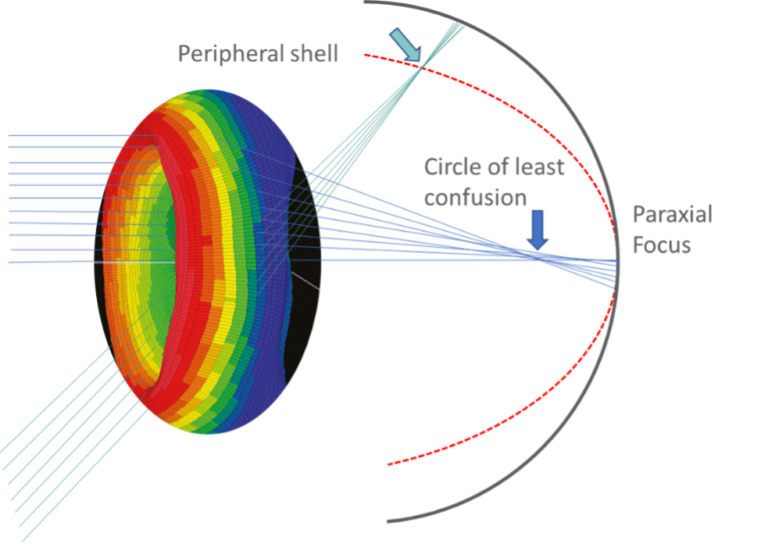
Figure 1. Peripheral defocus hypothesis is related to SA. Myopic peripheral shell is induced simultaneously with an increase of spherical aberration.
Almost all OK commercialized worldwide are similar to the original designs released 25 years ago for myopia refractive correction.

Figure 2. The fluorescein image of different orthokeratology brands is very similar
They produce a reduction in axial length growth in children of about 50%. However, these long-term “old” designs have limited efficacy in lower myopic or younger children.
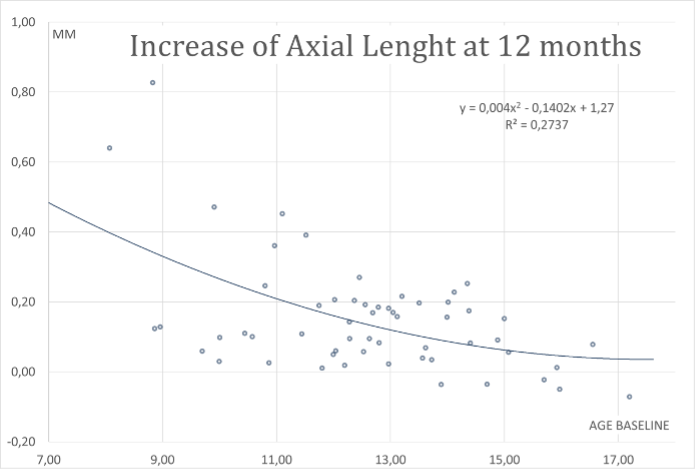
Figure 3. Typical axial length increases at one year regarding baseline age. Younger children wearing orthokeratology have a highest change in eye growth.
Currently, most ortho-k lenses feature four distinct zones that work together to achieve desired corneal topographical changes through tears and eyelid tension combined.
Researchers have investigated the clinical application of ortho-k lenses to determine how to enhance their myopia control effect by manipulating these lens parameters. Modifying ortho-k lens design to induce more beneficial visual signals has emerged as a new focus in myopia research. Various lens designs are prescribed to patients based on target myopia reduction and individual corneal conditions, such as corneal curvature, diameter, eccentricity value, and biomechanics.
With this latest research, we now know that optimizing the final optics induced on the cornea may improve the efficacy of myopia management. One of the best-known modifications is the reduction of the optical zone diameter, leading to a shrinking of what is called the treatment optic zone produced on the cornea8. This may increase the efficacy in slowing down axial length growth in children roughly by 50% to 85%, probably through optical signal modification.
Specific components of the lens design need to be modified or customized to get the optimal myopia control results. Research has shown that the refraction from the flattened central cornea and the steepened mid-peripheral cornea significantly impacts myopia control. The central and mid-peripheral cornea changes are primarily influenced by the design of the base curve (BC) and the reverse curve (RC). Relevant BC design parameters include the back optical zone diameter (BOZD) and the back optic zone radius (BOZR). Among these, BOZD is a determining factor for the width of the central treatment zone, while BOZR influences the flatness of the central cornea after wearing. Thus, current areas of study are the increase in the Jessen factor or compression factor obtained with an extra flattening of BOZR, the reduction of BOZD, and the change in the RC width or shape. In ortho-k lenses, the standard BOZD is typically designed to be around 6.0 mm. During ortho-k treatment, the central cornea will be flattened, which is referred to as the treatment zone (TZ) of approximately 4.0 ~ 5.0 mm. When light enters the eye through this area, it refocuses on the retinal macula, which can correct myopic refractive errors. During the fitting of ortho-k, BOZD refers to the pupil diameter to ensure a sufficiently large optical zone for maintaining standard visual quality9. However, our recent study evaluated the effect of BOZD on corneal reshaping in patients and found that a smaller BOZD resulted in a smaller TZ and a larger defocus ring (the corneal ring area where the refractive power exhibits a positive shift)10. We compared the efficacy of controlling the annual increase in axial length (AL) in myopic Caucasian children based on two parameters: the back optic zone diameter (BOZD) of the orthokeratology (OK) lens and plus power ring diameter (PPRD) or mid-peripheral annular ring of corneal steepening. The sample was divided into groups with BOZDs above or below 5.00 mm and the induced Plus Power Ring Diameter (PPRD) above or below 4.5 mm, and the relation to AL and refractive progression at 12 months was analyzed. Three subgroups were analyzed, i.e., plus power ring (PPR) inside, outside, or matching the pupil. Our results suggest that AL changes in subjects with smaller BOZDs decreased significantly regarding larger diameters. In subjects with a horizontal sector of PPRD falling inside the pupil, the AL increased less than matching or outside the pupil groups by a 76% lesser AL growth or 0.13 mm/year in absolute reduction.
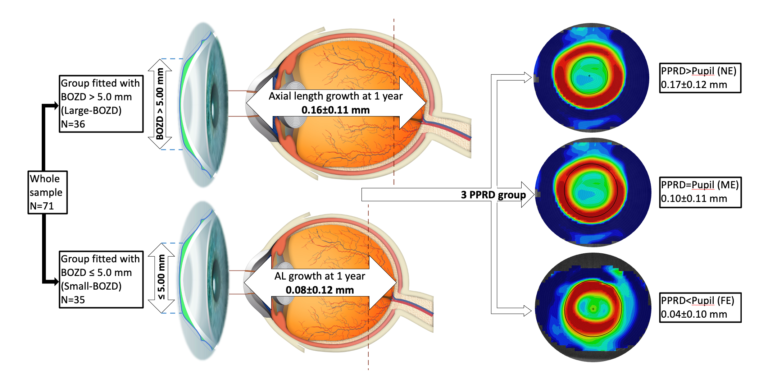
Figure 4. Results of our retrospective study10 were the group equipped with an optic zone diameter larger than 5.00 mm had a higher increase in myopia after one year. Furthermore, the group with the plus power ring placed inside the pupil showed the better axial length grow reduction.
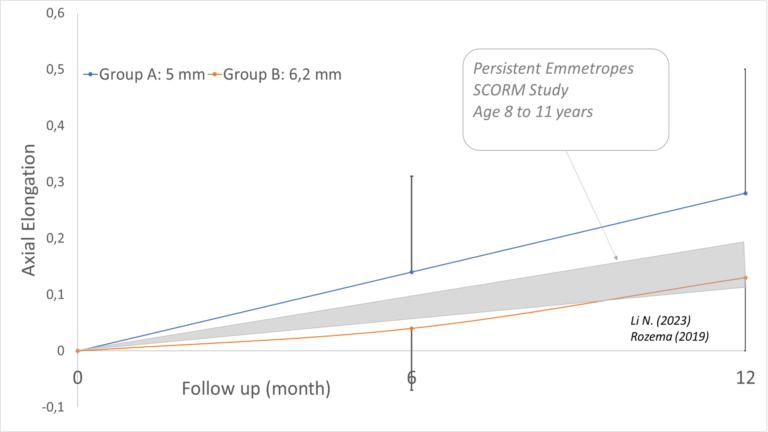
Figure 5. Comparison of the individuals with BOD reduced in orthokeratology and persistent emmetropes axial length increase at one year. Children with OK treatment with smaller BOD showed similar AL change after one year to emmetropes
The future looks promising, since those individuals that followed orthokeratology treatments with modified optic zones showed similar axial length growth to emmetropes. It is therefore important that practitioners and laboratories differentiate the types of lens designs used for simple myopia correction from those required for myopia management in children.