Introduction
In 2020, the COVID-19 pandemic wrought significant havoc on our healthcare system and daily lives. The implementation of public health measures, aimed at safeguarding the population, reshaped our professional landscape. We witnessed a surge in demand for contact lens fittings, coinciding with the return of our regular wearers seeking adjustments. These trends were primarily driven by the discomfort caused by mask-wearing, as well as the growing prevalence of remote work, which placed increased demands on near vision. Consequently, our workload escalated, necessitating the restructuring of our clinics for enhanced efficiency.
Concurrently, as our contact lens fitting consultations surged, we observed a swifter discontinuation of older contact lens models by some manufacturers. However, discontinuing a lens type also entails the responsibility of providing wearers with new models that cater to their vision and comfort requirements. In this demanding environment, characterized by heightened activity, we contemplate the possibility of unearthing valuable solutions through university research.
Case report
Allow me to illustrate how such research, requiring no additional equipment beyond what is already available in our clinics, could streamline the process of refitting long-time wearers while minimizing the time spent in the chair.
Consider the case of a 49-year-old male, a long-time contact lens wearer, who previously reported optimal comfort with his lenses:
Original Lens
OD -4.75 (-1.25) 130° Diam : 14.50 Bc : 8.50
OS -4.00 (-1.25) 90° Diam : 14.50 Bc : 8.50
Visual acuity was good with OD 20/20 (1.0) and OS 20/20 (ODS 20/20)
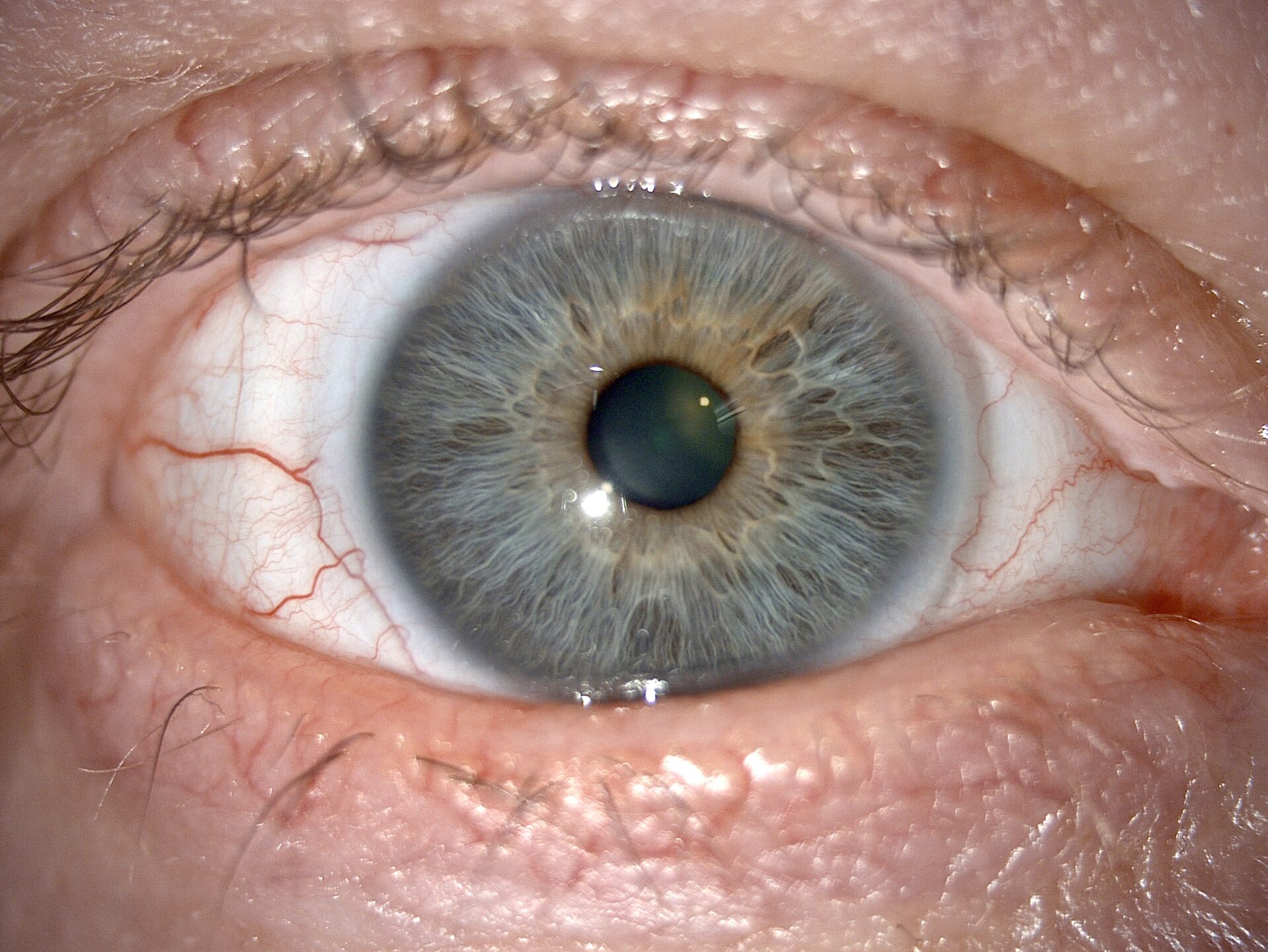
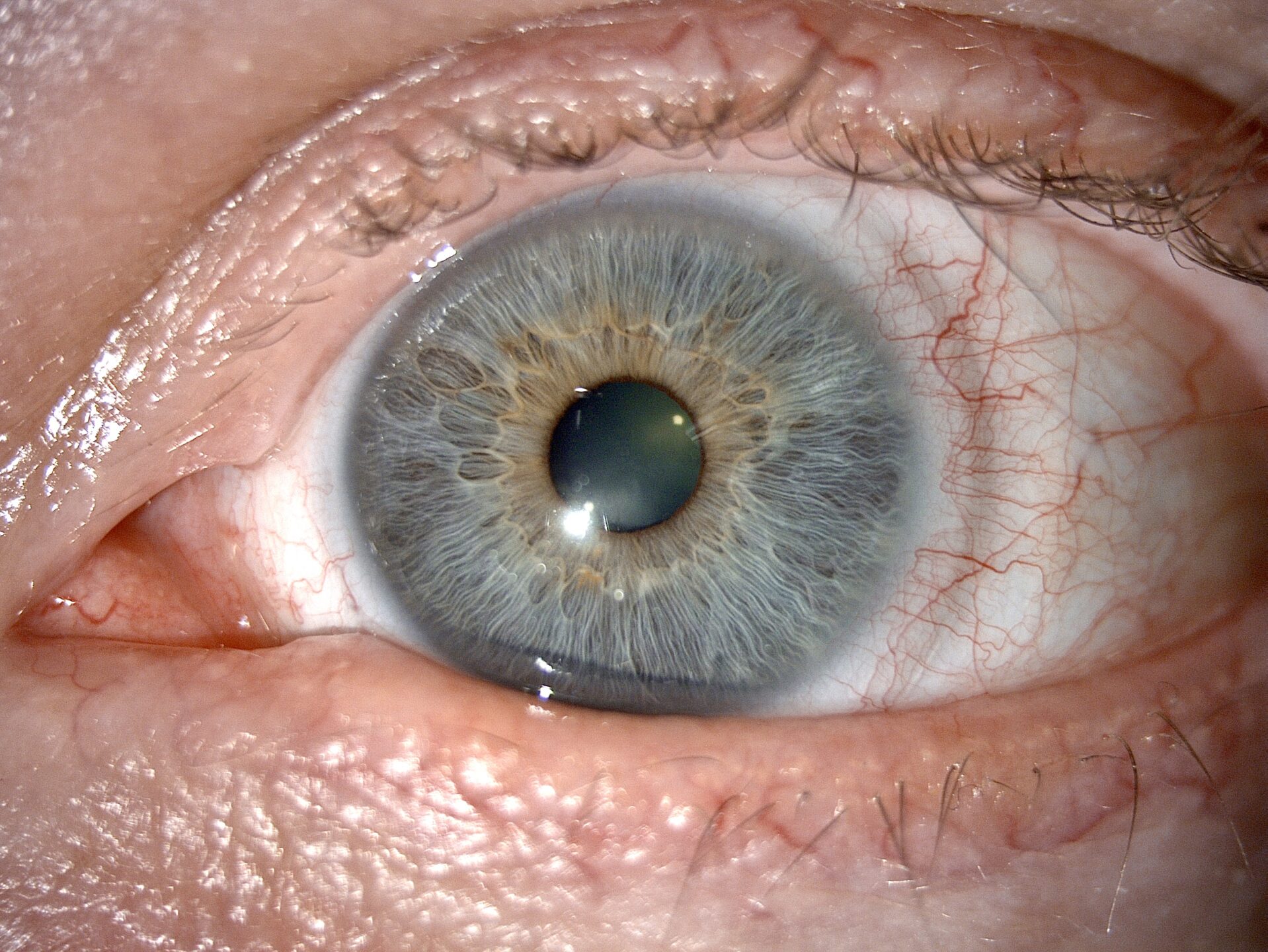
Fitting: Optimal, with excellent lens centering. A slight movement was observed during ocular versions, but a good return to the push-up position. Lens surface condition remained good after 11 hours of continuous wear.
However, the reason for his appointment was the lens type the patient was currently wearing successfully was going to be discontinued, necessitating the search for an alternative. He had already sought assistance from his longstanding fitter but without success.
Subsequently, we examined without lenses:
Trial (and error)
Here we find the trials done in the context of refit. It is important to note that these tests were repeated for the writing of this report, as we did not have access to the previous observations.
1st Trial Lens:
OD -4.75 (-1.25) 130° Diam : 14.50 Bc : 8.60
OS -4.00 (-1.25) 90° Diam : 14.50 Bc : 8.60
Result: Excessive lens movement and visual instability. The lenses cannot be worn longer than one hour.
2nd Trial Lens:
OD -4.75 (-1.25) 130° Diam : 14.50 Bc : 8.60
OS -4.00 (-1.25) 90° Diam : 14.50 Bc : 8.60
Result: Improved lens stability, but excessive movement persisted. The discomfort was reported after a few hours of wear, rendering this lens unsuitable as a substitute for the his previous lenses.
3rd Trial Lens:
OD -4.75 (-1.25) 130° Diam: 14.50 Bc: 8.70
OS -4.00 (-1.25) 90° Diam: 14.50 Bc: 8.70
Result: Even though the surface of this lens appeared to be greatly improved, the dynamic behavior remained unacceptable. The patient even noted that, during trials, the entire lens slid over the cornea.
Making a Change
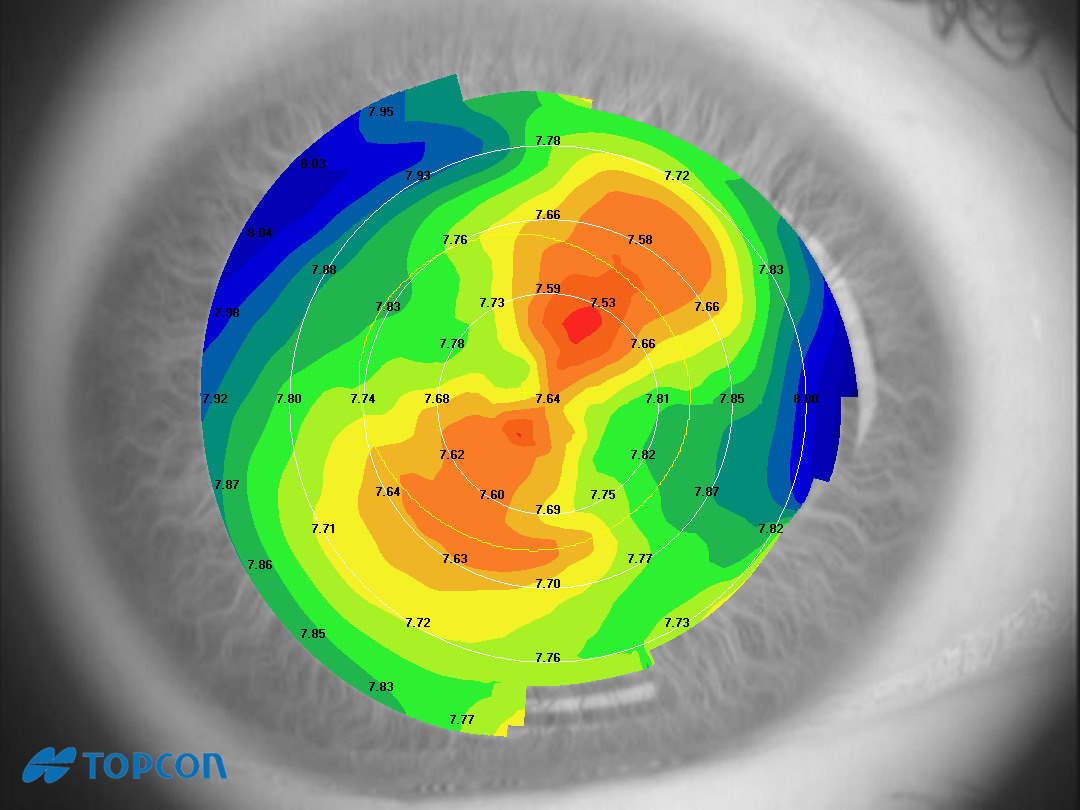
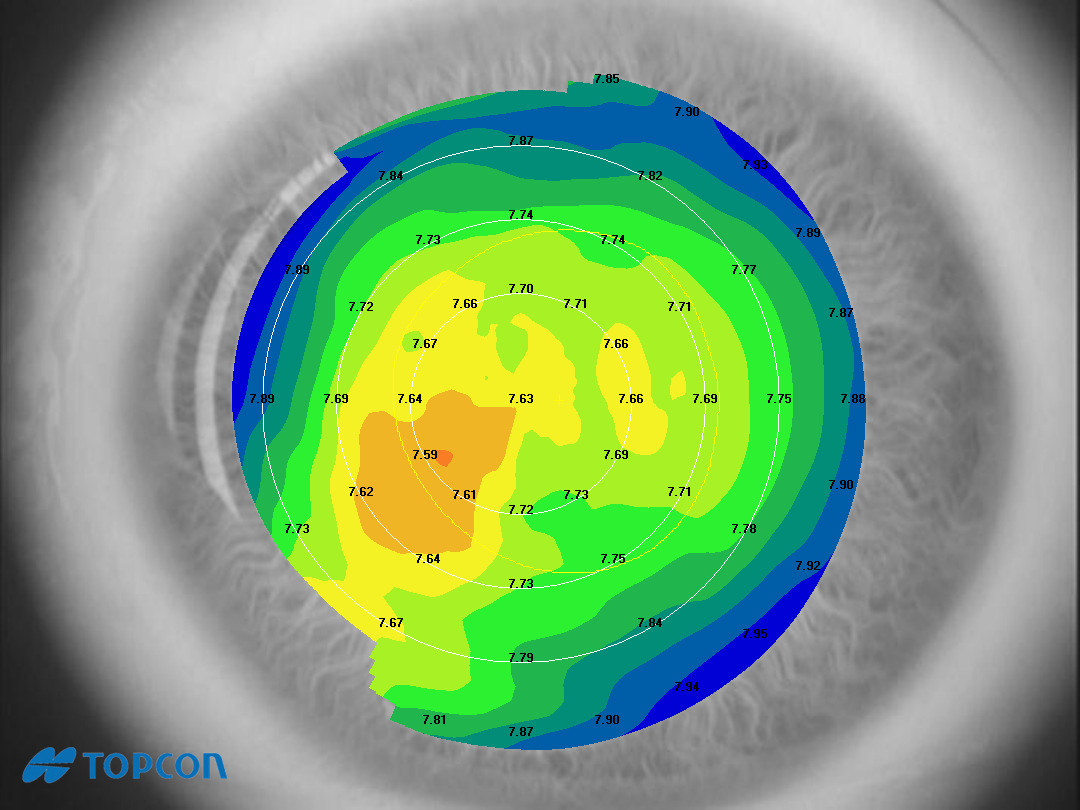
In a fresh perspective on this refitting challenge, we turned to the latest research insights. In January 2021, van der Worp et al. introduced a CL-SAG analysis for today’s most popular soft lenses. Notably, the original lens design exhibited the highest SAG in the chart at 4157 µm. This aligns with historical practices of using this lens for steeper corneas specifically, as confirmed by this research.
It is therefore interesting to compare the previously used unsuccessful lenses with the CL-SAG value of his previous successful lens:
For the first trial lens, the SAG difference is 188 µm.
For the second trial lens, the SAG difference is 277 µm.
For the third trial lens, the SAG difference is 297 µm.
This correlation with clinical analysis is striking. Regardless of the radius of curvature and lens diameter (the only parameters easily accessible to the fitter), it is evident that the sagittal height of a soft lens significantly influences its behavior on the wearer’s eye.
With this revelation, we opted to select a lens with the closest SAG to the original lens. Consequently, we ordered the following lenses for trial:
4th Trial Lens:
OD -4.75 (-1.25) 130° Diam: 14.50 Bc: 8.40
OS -4.00 (-1.25) 90° Diam: 14.50 Bc: 8.40
According to van der Worp et al., the CL-SAG of the fourth trial lens is 4153 µm. Compared to the historical lens, the SAG difference is only 7 µm.
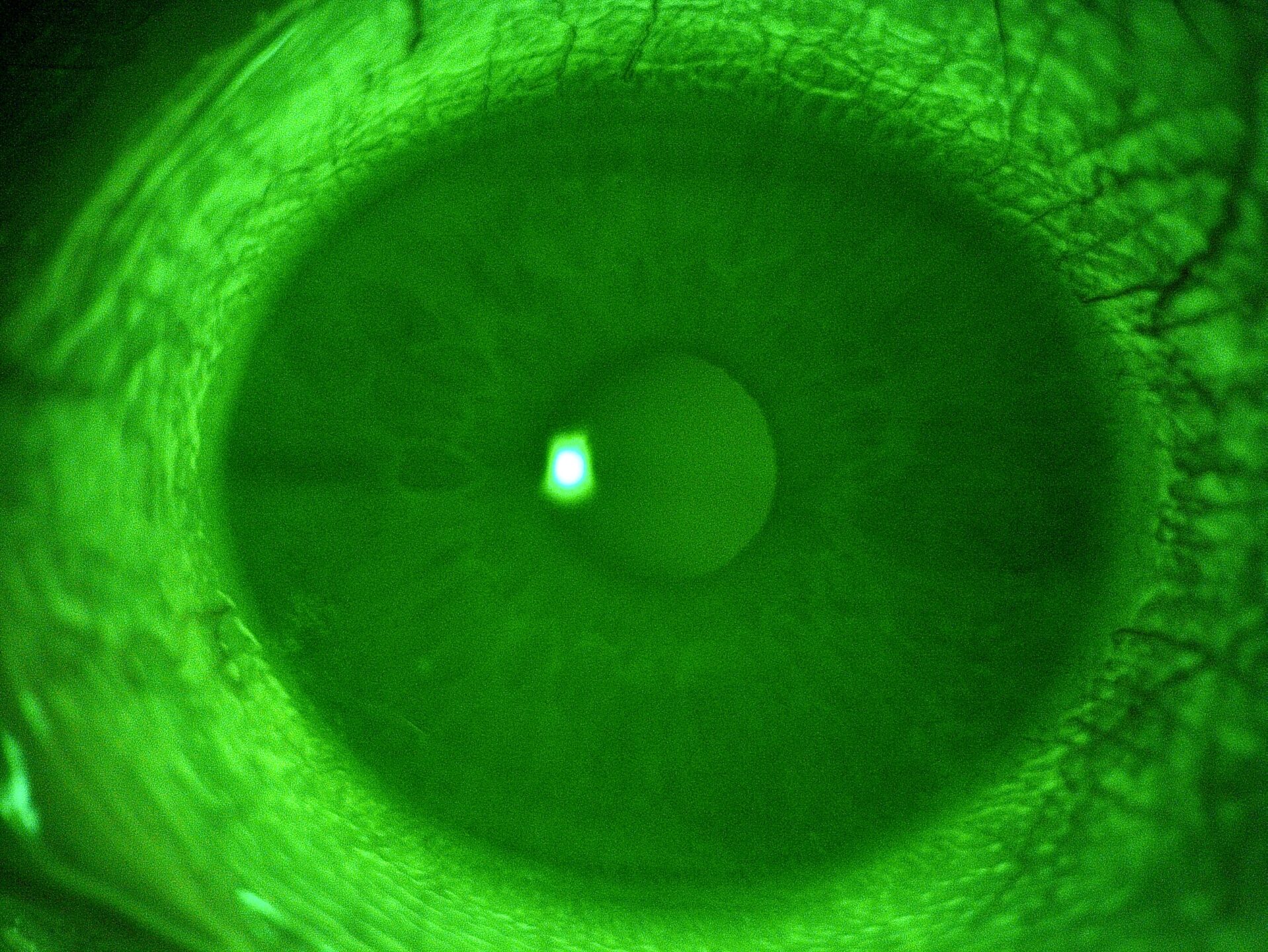
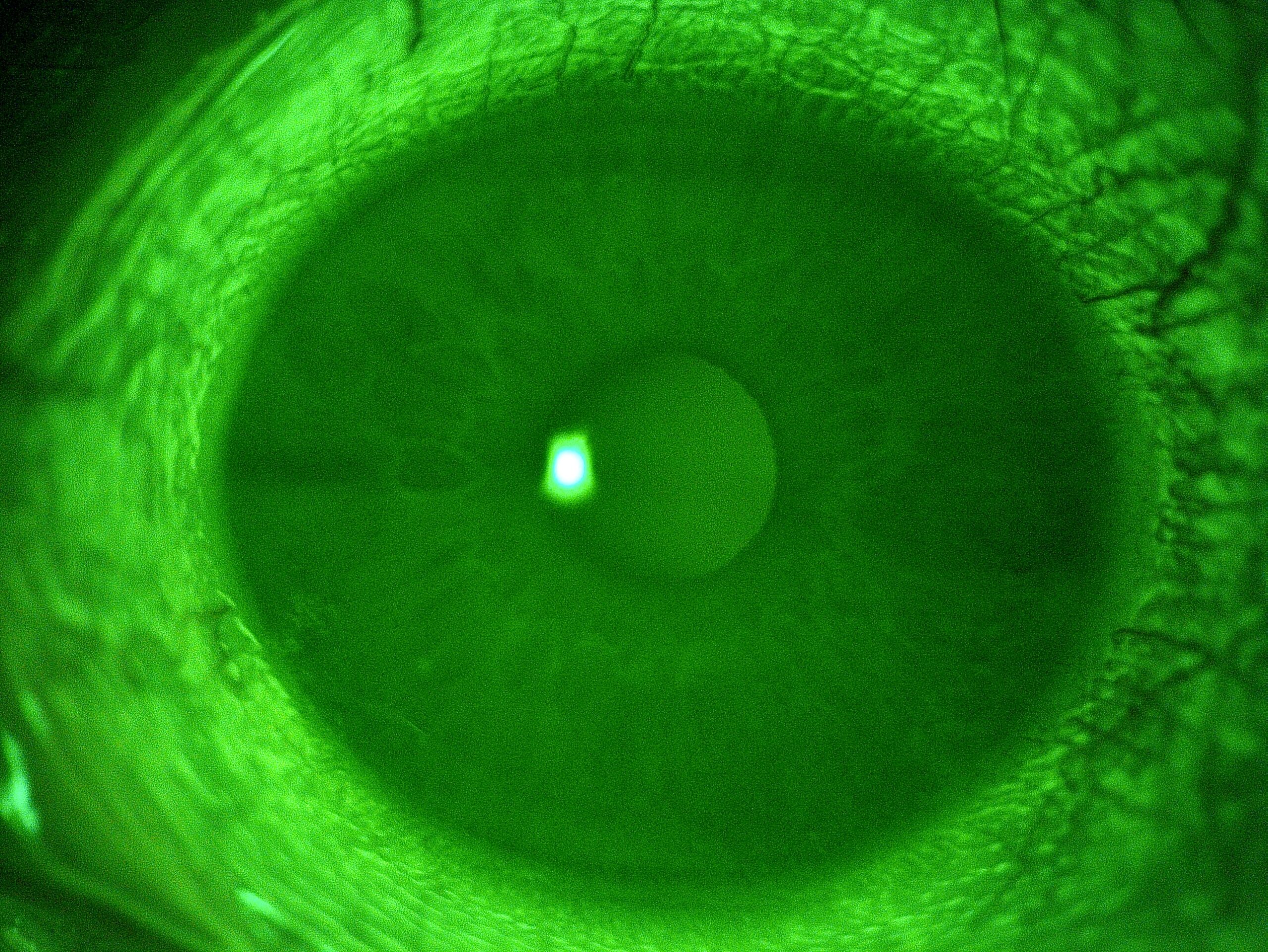
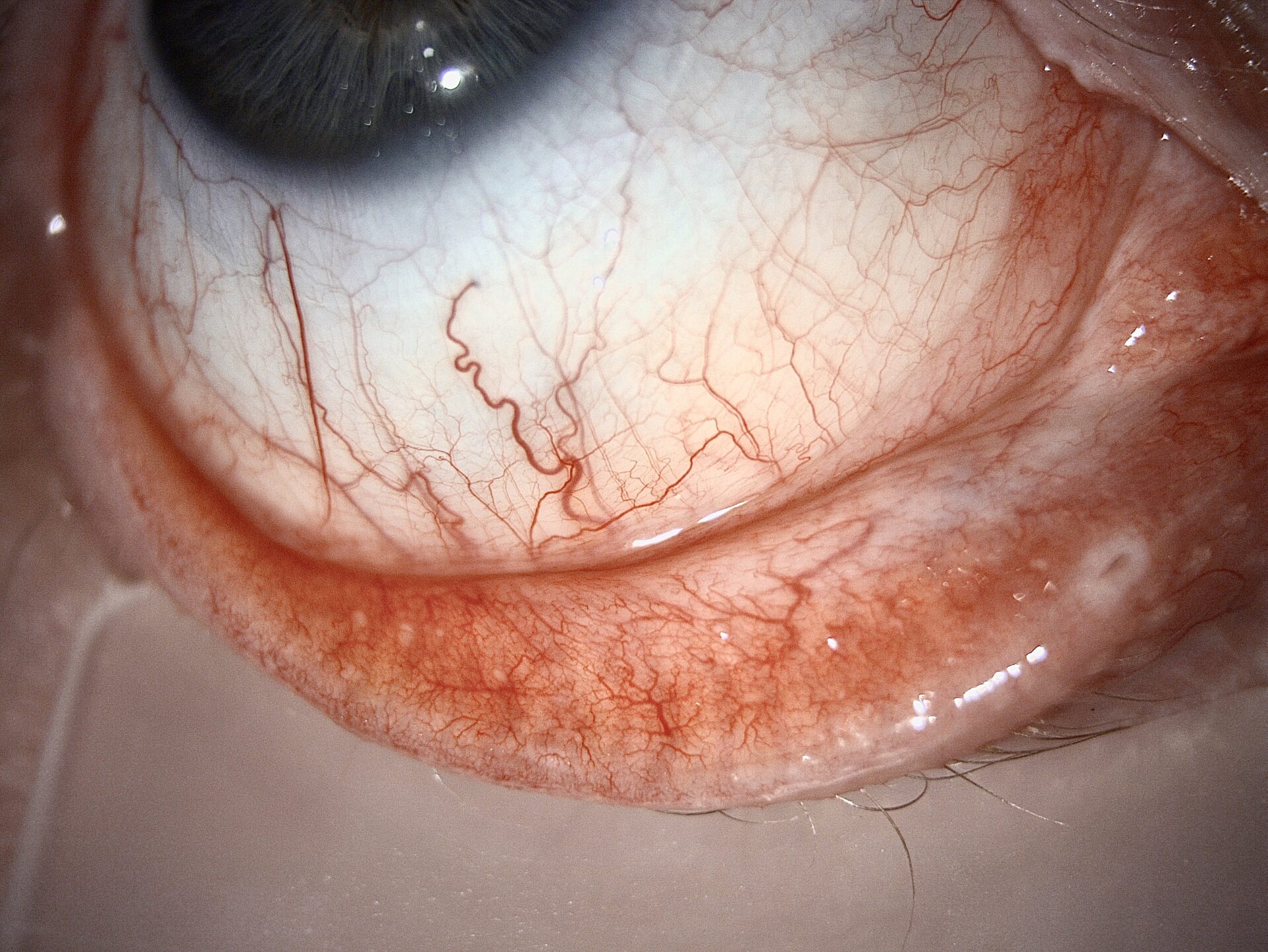
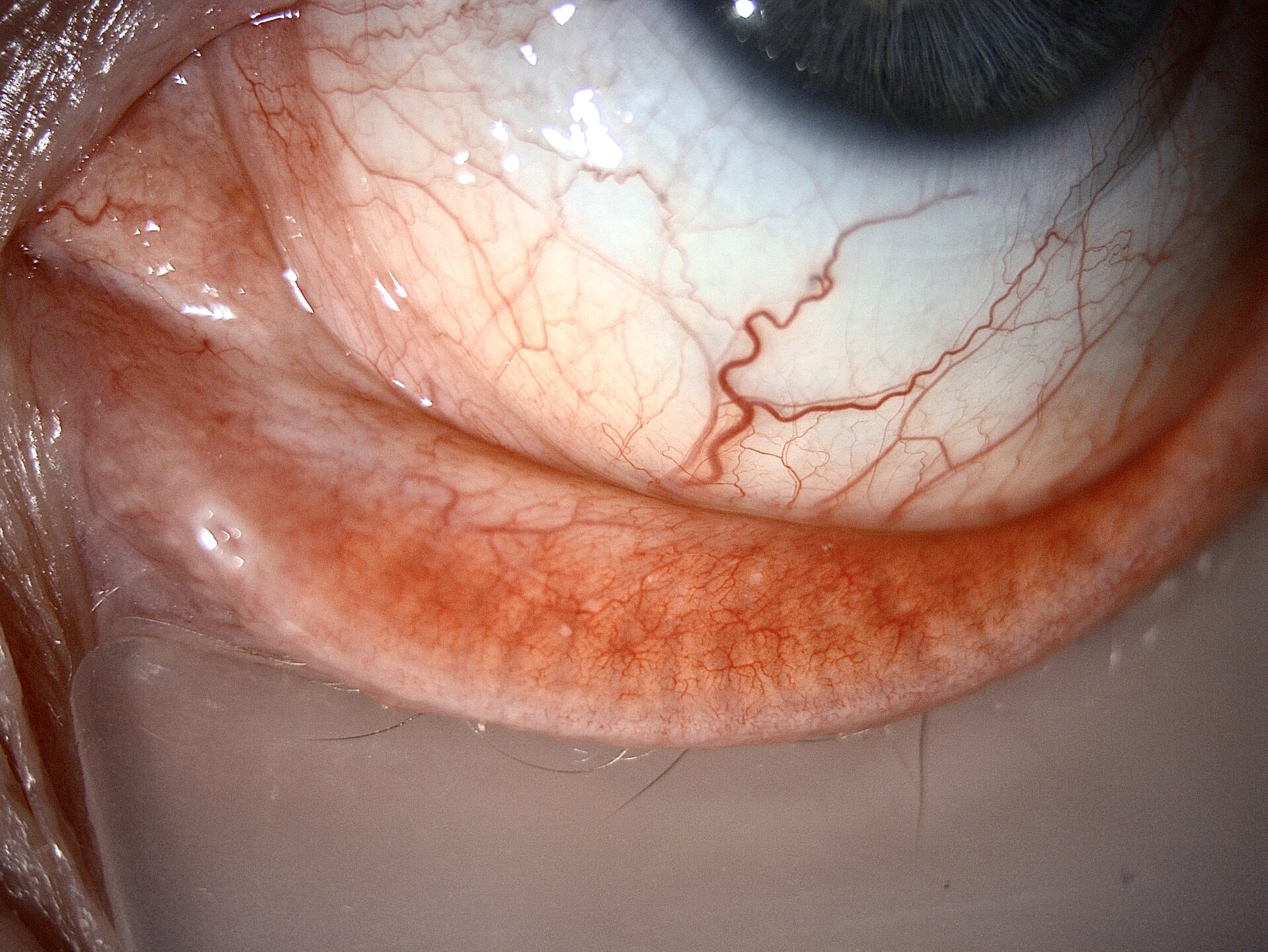
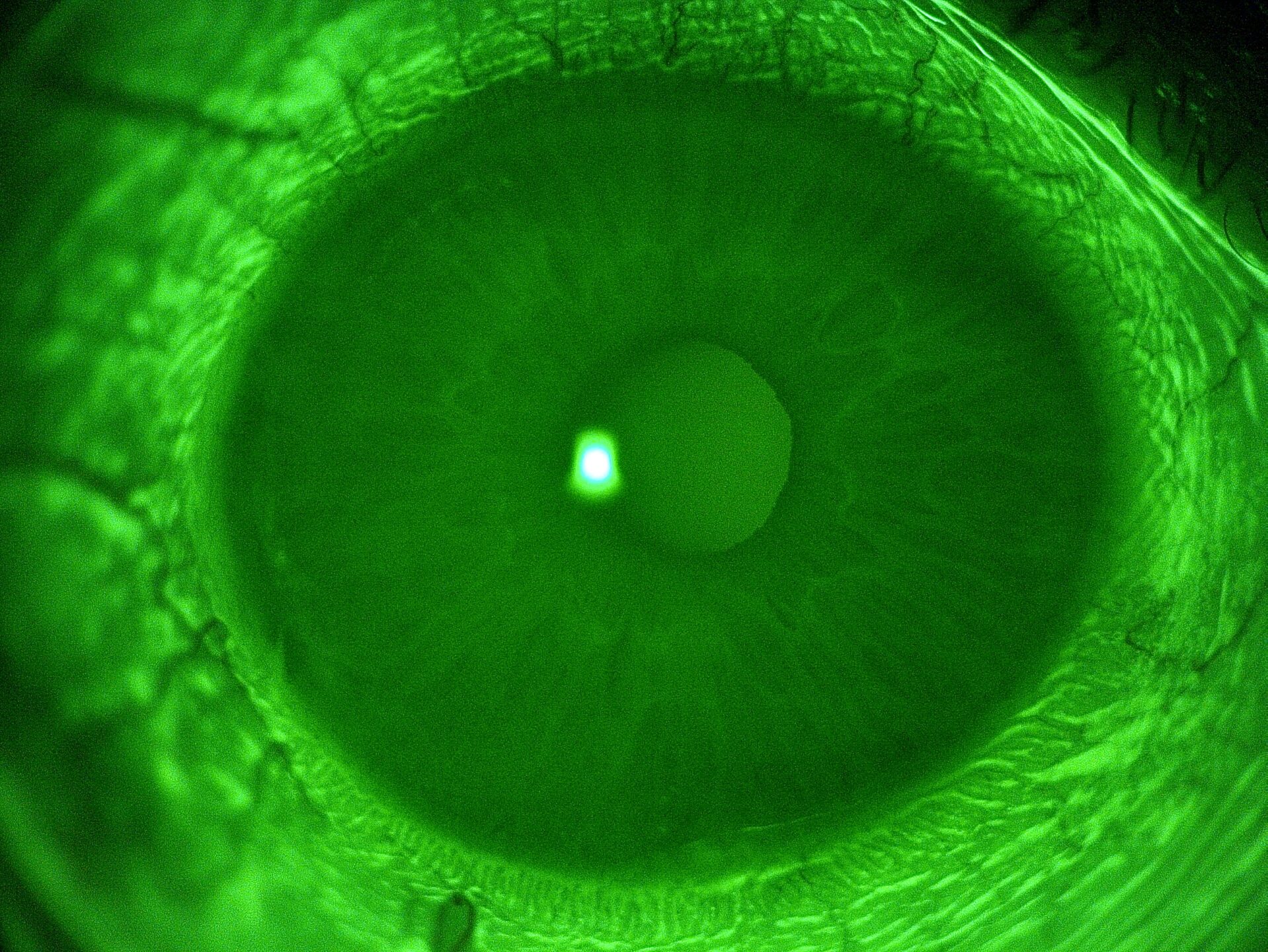
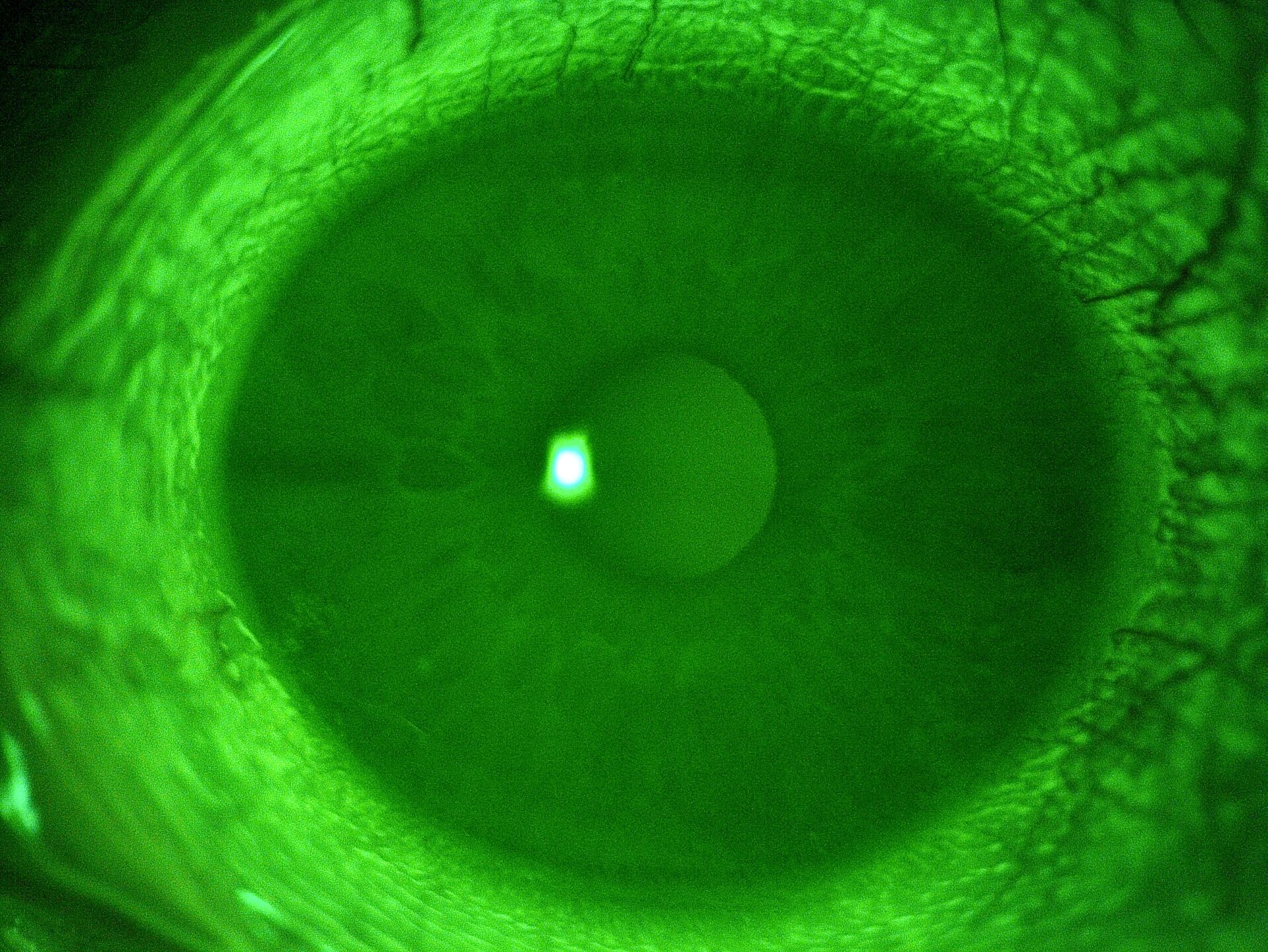
After one day’s wear, the patient reported regaining the comfort he had with his old lenses. The examination revealed a well-centered lens with good mobility and movement back to the standard location was observed as is desired. The surface condition remained unchanged, even after extended wear and when the lenses are removed, fluorescein examination reveals no staining.
Closing Remarks
In summary, this case underscores how university research, utilizing existing clinic equipment, can rapidly identify a first-choice replacement lens. In this instance, it could have averted three unsuccessful trials, saving considerable consultation time. It also prompts us to reconsider our lens selection methodology, both initially and for optimization purposes. Moreover, this case report reaffirms that there is no direct correlation between the diameter/base curve and the actual behavior of the worn lens on-eye.
This also prompts us to reconsider the significance of made-to-order soft contact lenses, which continue to be an effective tool for controlling the sagittal heights of the fitted lenses. In this case, we prescribed a daily replacement lens, another option would have been to consider a customised soft lens that matched the SAG of the original lens.
It would therefore be interesting to pursue this work to complete the lens types analyzed with new lenses that come to the market and facilitate the use of this work at a time when the notions of sagittal height are gaining more attention with the increasing popularization of scleral lens fitting.