
Scleral lenses have an astounding ability to provide patients with the gift of sight, often allowing them to regain their lives. With keratoconus (KCN) being the most common indication for scleral lenses, patients often experience a significant improvement in visual function with wear.1
It is well-understood that, by providing a smooth refractive surface, scleral lenses have the capacity to correct for visual distortions caused by corneal irregularity. Scleral lenses also correct for some degrees of higher order aberrations (HOAs); however, patients may continue to experience visual distortions from residual HOAs. A patient who continues to be affected by HOAs with scleral lens wear may report symptoms of “ghosting”, “shadowing”, or “doubling” of their vision.2–4 Wavefront-guided correction allows for customized optics at the front surface of contact lenses (CLs), including scleral lenses to correct for a patient’s specific HOA profile.2
Prosthetic replacement of the ocular surface ecosystem (PROSE) is a treatment that uses a highly customizable scleral lens, deemed a prosthetic device (PD), for the management of irregular corneal shape and ocular surface disorders. The PD used in PROSE treatment functions like that of a scleral lens, as it is made of a clear rigid-gas permeable material that is filled with preservative-free saline and applied to the ocular surface and rests on the sclera. With PROSE, customizability in correction for HOAs through wavefront-guided optics is possible. Other scleral lens designs have demonstrated capability to offer wavefront-guided correction as well.5
With the exponential growth of scleral lens wear and technological advances in the industry in recent years, there has been a reduced need for corneal transplants.6 As HOA correction with scleral lenses through wavefront-guided optics becomes increasingly available, practitioners will be able to offer enhanced visual function, which could potentially further reduce the need for corneal transplants in the KCN population.
This report reviews the case of a patient with keratoconus, who had limitations in vision due to residual HOAs. Wavefront-guided optics corrected for their residual HOAs, which significantly improved the patient’s visual function and deterred their interest in pursuing invasive corneal transplant surgery.
Case Report
Patient History
A 54-year-old Caucasian with ocular history of bilateral KCN presented to BostonSight for follow-up. They initially underwent PROSE treatment in 2017 and continued with daily wear of their PROSE devices for visual function. Prior to wearing their PROSE devices, they had tried and failed with all varying types of CL modalities including corneal gas permeable (GP) lenses, hybrid CLs, and other scleral lenses.
The patient’s profession in health care and management had a high vision demand. They were motivated to better their vision to improve their daily visual function. The patient had been advised in the past that should vision improvement be limited with specialty lenses, they may have to consider a corneal transplant. Although this was a notion which the patient was able to forgo for years since their diagnosis, they anticipated that this may be the next appropriate step in their vision journey to restore their visual function so they may meet their daily visual demands.
Case Presentation
At the patient’s routine follow-up appointment, their chief complaint was that of persistent “blur”, “doubling”, and “ghosting” of vision with their PROSE devices, worst at nighttime and with left worse than right eye.
Entering best corrected visual acuity (BCVA) with PROSE:
OD: 20/40+1 (PH 20/20-2)
OS: 20/50 (PH 20/25+2)
Presenting PROSE device parameters:
OD: 18.5mm OAD/ 8.00 BC/ 3.03 sag/ +2.37 -0.50 x 005/ 0.3 CT/ quadrant-specific design
OS: 18.5mm OAD/ 8.00 BC/ 3.03 sag/ +2.50 -0.75 x 030/ 0.3 CT/ quadrant-specific design
The fit for each PD was found to have adequate corneal and limbal clearance throughout. No edge staining was noted on the conjunctiva after PD removal for either eye; however, there was moderate rebound hyperemia which was concerning for suction with PD wear.
Slit lamp examination (SLE) corneal findings showed mild apical thinning and steepening, with Vogt’s striae and positive presence of a Fleischer ring for each eye. No corneal scarring or neovascularization was noted for either eye. The patient’s intraocular pressure (IOP) with Goldmann applanation tonometry (GAT) was 15 for each eye. All other findings, including pupils, and extraocular motility (EOM) were found to be normal. Posterior segment findings as reported from a recent dilated fundus examination (DFE) from her primary eye care provider, a corneal specialist, showed normal posterior segment findings. The patient’s medical history and systemic medications were noncontributory. They were not using any prescribed or over-the-counter ophthalmic medications.
The patient’s visual complaints were consistent with that of residual HOAs. To quantify the degree of HOAs with her presenting PDs, corneal aberrometry scans were obtained for each eye. Aberrometry scans confirmed residual HOAs, left eye worse than right (Figure 1).
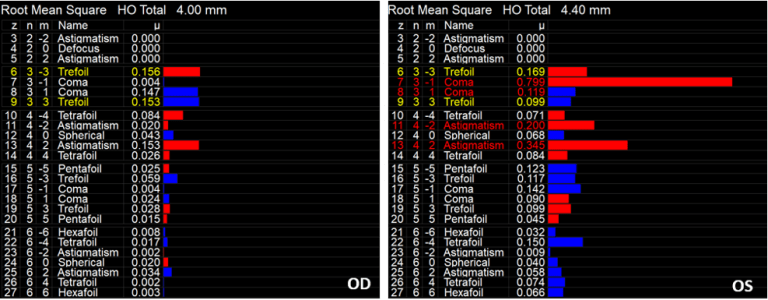
Figure 1: iTrace aberrometry scans demonstrating residual HOAs with patient’s presenting PROSE device for the right (OD) and left (OS) eye. Residual HOAs were more pronounced for the left than right eye, consistent with patient’s chief complaint.
After further discussion of clinical findings, the patient confirmed symptoms of suction with lens wear including aching and soreness as well as rebound redness after lens removal for both eyes. The decision was made to modify the fit for both eyes, with the goals of improving comfort by mitigating suction and optimizing vision by attempting to correct for the residual HOAs.
Refitting/ PROSE Retreatment
With PROSE retreatment, the diameter was increased by 0.5mm for both eyes to provide a wider haptic edge to better distribute the weight of the device for each eye (Figure 2). This was done to reduce the amount of suction with prolonged lens wear. Each lens was also converted from a quadrant-specific haptic design to an eight-meridian haptic design for optimal customization and fitting. With retreatment, the patient’s rebound hyperemia and complaints of discomfort after PD removal were resolved.
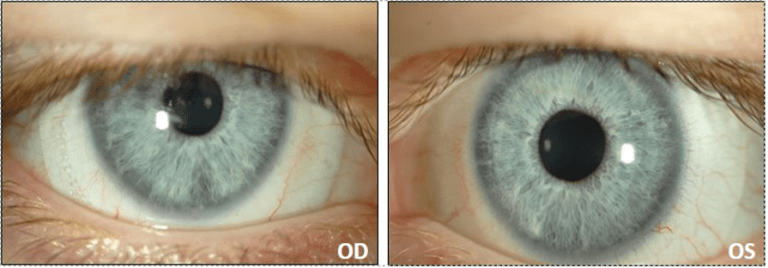
Figure 2: Finalized PROSE fit for the right (OD) and left eye (OS) in 19.0mm designs.
HOA Correction with PROSE
Once the fit was stable for each eye, we pursued HOA correction. Aberrometry scans over the patient’s optimized PDs were acquired under dilated conditions to better quantify the degree of HOAs in scotopic conditions.
The aberrometry data was incorporated into the PROSE design for each eye. A repeat refraction was performed over the wave-front guided PROSE devices, which was included in the final design. The patient reported significant improvement in daily visual function, with improvement of “ghosting” in the left eye and complete resolution of ghosting for the right eye.
BCVA with final wave-front guided PROSE:
OD: 20/20-1
OS: 20/25-1
Final PD Parameters:
OD: 19.0mm OAD/ 8.00 BC/ 3.03 sag/ +2.00 sph/ wavefront optics/ 0.3 CT/ eight-meridian design
OS: 19.0mm OAD/ 8.00 BC/ 3.03 sag/ +2.50 sph/ wavefront optics/ 0.3 CT/ eight-meridian design
Repeat aberrometry scans were obtained over the final wavefront corrected PDs which confirmed significant reduction in HOAs. The most notable improvement was observed for coma, which can be the most visually significant in KCN patients (Figures 3 and 4).
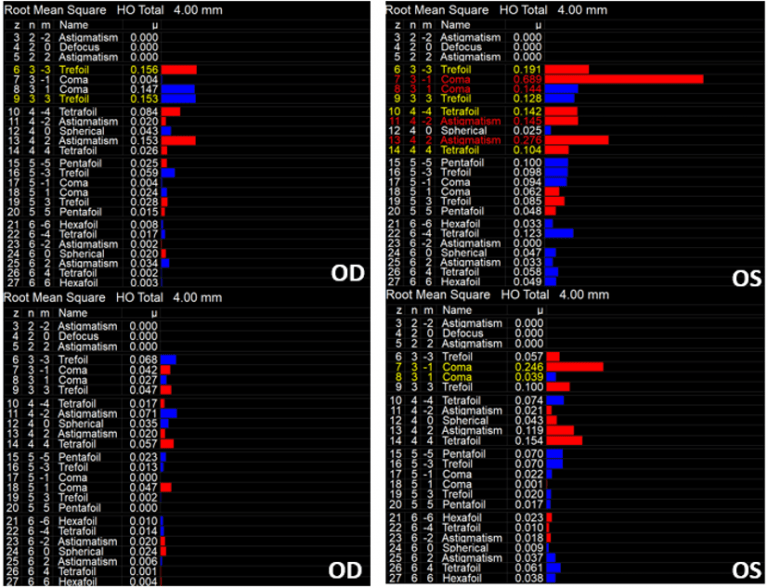
Figure 3: iTrace aberrometry scans with patient’s presenting PROSE devices (top) for the right (OD) and left (OS) eye, compared to patient’s finalized PROSE devices (bottom) for the right (OD) and left (OS) eye.
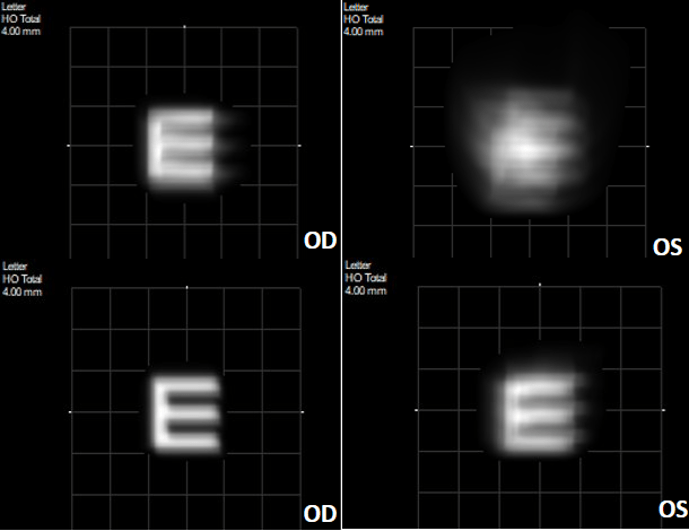
Figure 4: iTrace visual function analyzer (VFA) scan demonstrating the vision quality with the patient’s presenting right (OD) and left (OS) PD (top) versus the patient’s finalized wavefront-guided devices (bottom). There is a notable improvement in quality of vision based on the VFA for each eye.
Discussion
Higher Order Aberrations and Scleral Lenses
Bringing wavefront-guided scleral lenses involves various considerations, including determining who may be an appropriate candidate. The HOA profile of each patient is as unique as their fingerprint – no two eyes are the same. The recipe for HOA correction with scleral lenses has four key ingredients:
- Patient must have some vision improvement potential.
- Improved vision with pinhole.
- Symptoms of HOAs which can be quantified as HOAs based on aberrometry scans.
- Access to an aberrometer, with reliable aberrometry scans.
- A rotationally and tangentially stable scleral lens design.
- Much like the need for a toric soft CL to be stable to function properly, a wavefront-guided scleral lens also needs to be stable while on the eye.
- Access to a wavefront-guided lens design with an appropriate manufacturing lab.
Conclusion
Although specialty CLs including scleral lenses can greatly improve visual function and correct for some degrees of HOAs, residual HOAs can haunt patients’ visual function as they experience symptoms like blur, distortion, doubling, shadowing, glare, and ghosting. Correcting for HOAs can further improve visual function in patients suffering from KCN; therein, potentially further reducing the need to pursue invasive corneal surgery such as penetrating keratoplasty.
As technological advances continue to unfold and HOA correction through wavefront-guided technology becomes increasingly available to practitioners, the future is looking increasingly bright for patients.
1. Schornack MM. Scleral lenses: A literature review. Eye Contact Lens. Published online 2015. doi:10.1097/ICL.0000000000000083
2. Sabesan R, Johns L, Tomashevskaya O, Jacobs DS, Rosenthal P, Yoon G. Wavefront-guided scleral lens prosthetic device for keratoconus. Optom Vis Sci. 2013;90(4):314-323. doi:10.1097/OPX.0b013e318288d19c
3. Chalita MR, Xu M, Krueger RR. Correlation of Aberrations with Visual Symptoms Using Wavefront Analysis in Eyes after Laser in situ Keratomileusis. J Refract Surg. 2003;19(6):682-686. doi:10.3928/1081-597X-20031101-13
4. Naderan M, Shoar S, Kamaleddin MA, Rajabi MT, Naderan M, Khodadadi M. Keratoconus Clinical Findings According to Different Classifications. Cornea. Published online 2015. doi:10.1097/ICO.0000000000000537
5. Marsack JD, Ravikumar A, Nguyen C, et al. Wavefront-guided scleral lens correction in keratoconus. Optom Vis Sci. Published online 2014. doi:10.1097/OPX.0000000000000275
6. Koppen C, Kreps EO, Anthonissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral Lenses Reduce the Need for Corneal Transplants in Severe Keratoconus. Am J Ophthalmol. Published online 2018. doi:10.1016/j.ajo.2017.10.022
7. Chahal JS, Heur M, Chiu GB. Prosthetic Replacement of the Ocular Surface Ecosystem Scleral Lens Therapy for Exposure Keratopathy. Eye Contact Lens. 2017;43(4):240-244. doi:10.1097/ICL.0000000000000265
Thank you to Bita Asghari for contributing to Global Insight.


