Background:
Ectodermal Dysplasias (ED) are genetic conditions affecting the development of skin, hair, teeth, nails, and sweat glands1. Ocular findings include lacrimal drainage obstruction and hypoplasia, punctal agenesis, distichiasis, trichiasis, meibomian gland alterations and ankyloblepharon with sequelae of chronic dry eye2,3.
Complications include chronic ocular pain, neurotrophic keratitis, and corneal opacification4. Among other treatments, scleral lenses (SL) can optimize vision and maintain the health of the ocular surface. This case series highlights two patients with ED successfully fit with large diameter SLs.
Case 1:
42-year-old Caucasian female presented for dry eye and scleral lens consultation. H/o ED with malformation of nasolacrimal ducts OU, herpes zoster keratitis OU in 2017 with corneal scarring OS > OD. Habitual scleral lens use with inadequate fit due to corneal touch.
Quadrant specific SLs were designed with a larger diameter and increased central clearance, to be used in conjunction with autologous serum tears to improve the ocular surface. After 2 months of wear, corneal punctate staining fully resolved.
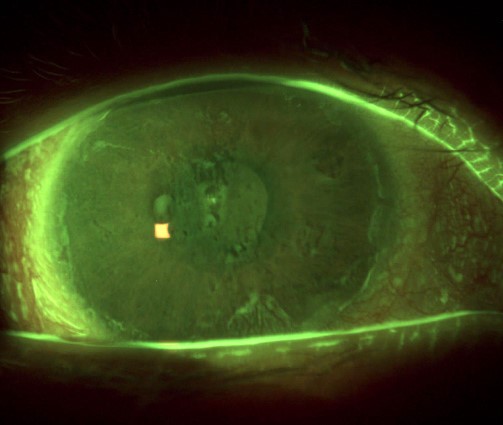
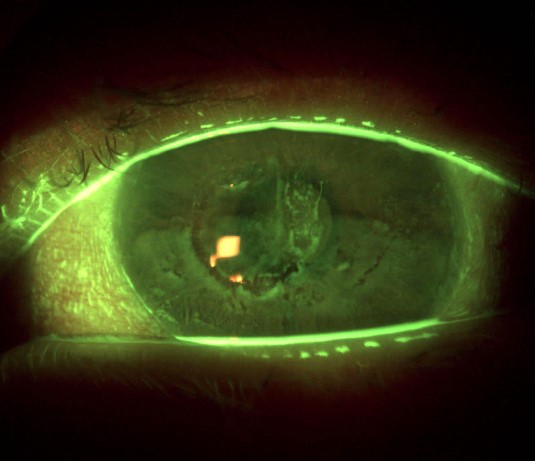
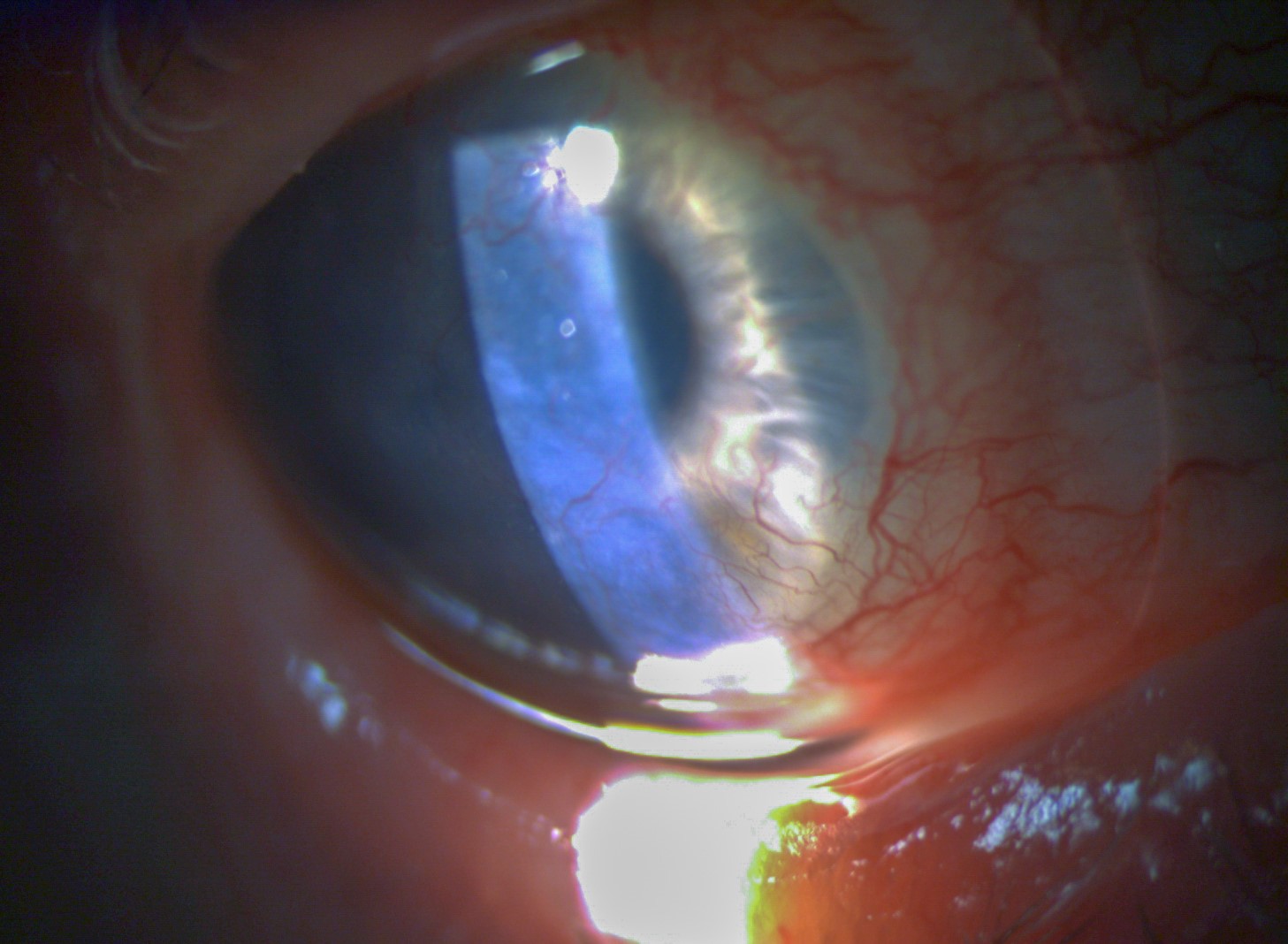
Figures 1a and 1b: Slit lamp examination of the cornea OD/OS: Mixed NaFl staining secondary to lens touch. Corneal irregularity due to central corneal scarring, thinning, and neovascularization. Diffuse bulbar conjunctival staining secondary to exposure keratopathy.
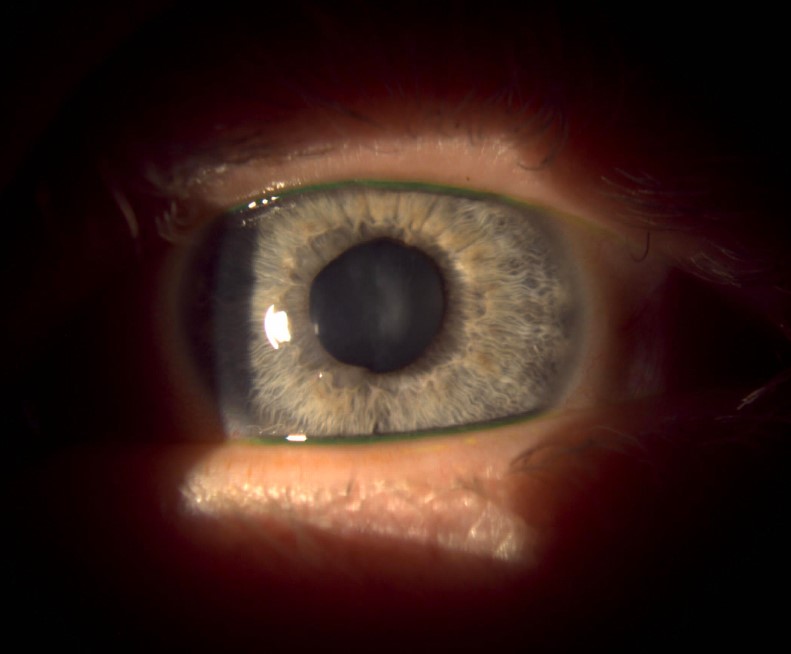
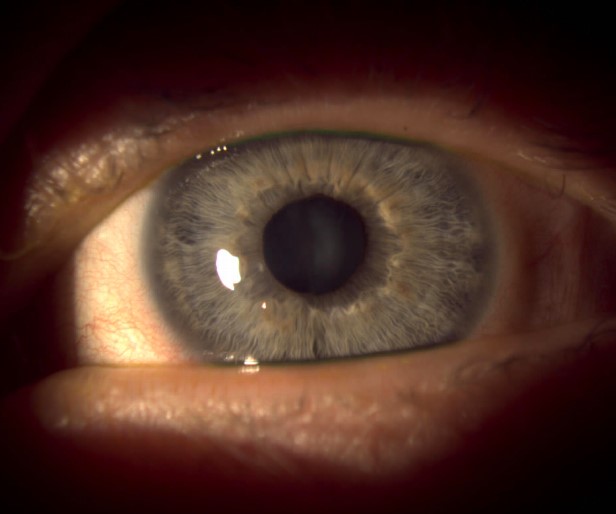
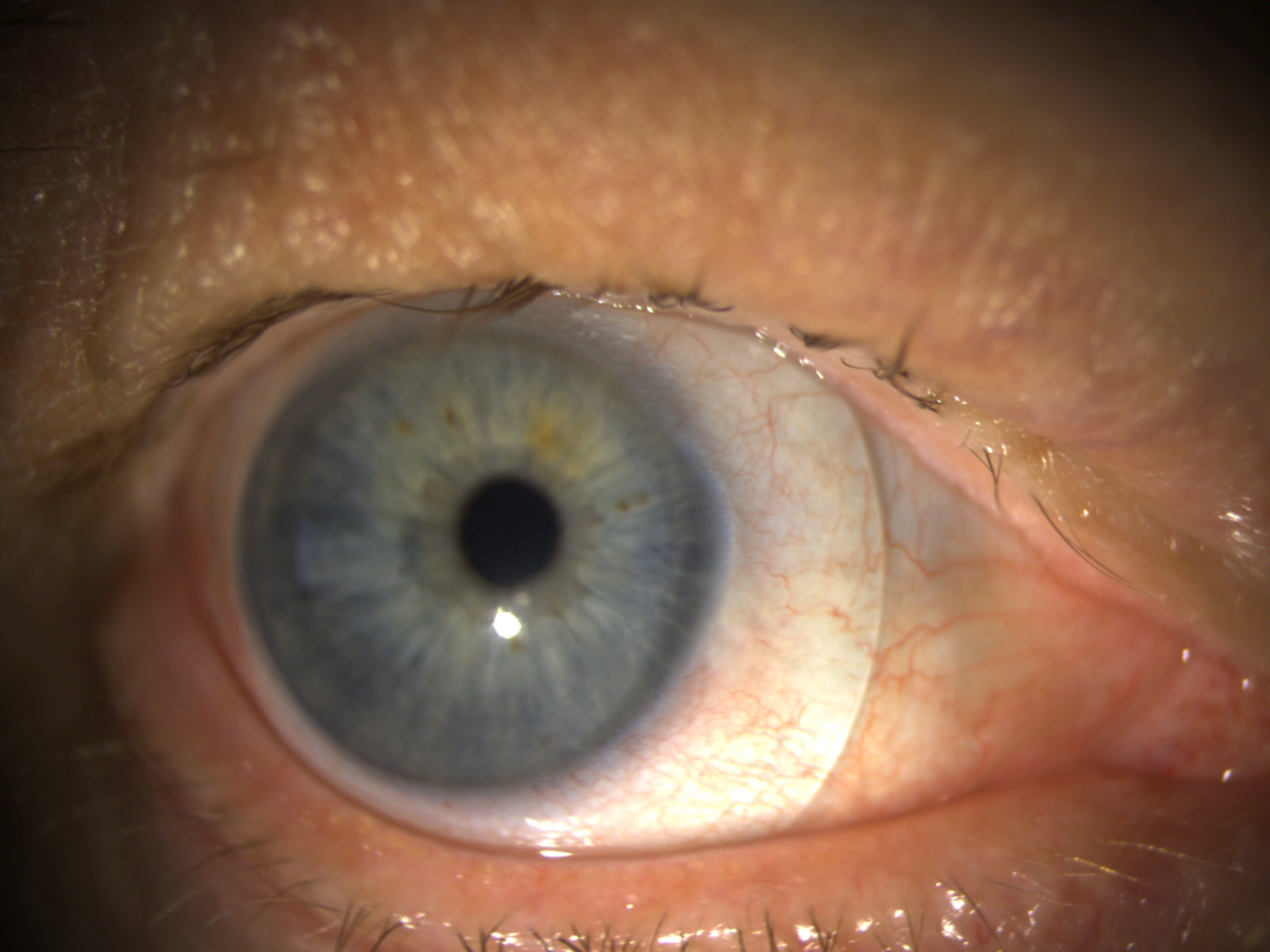
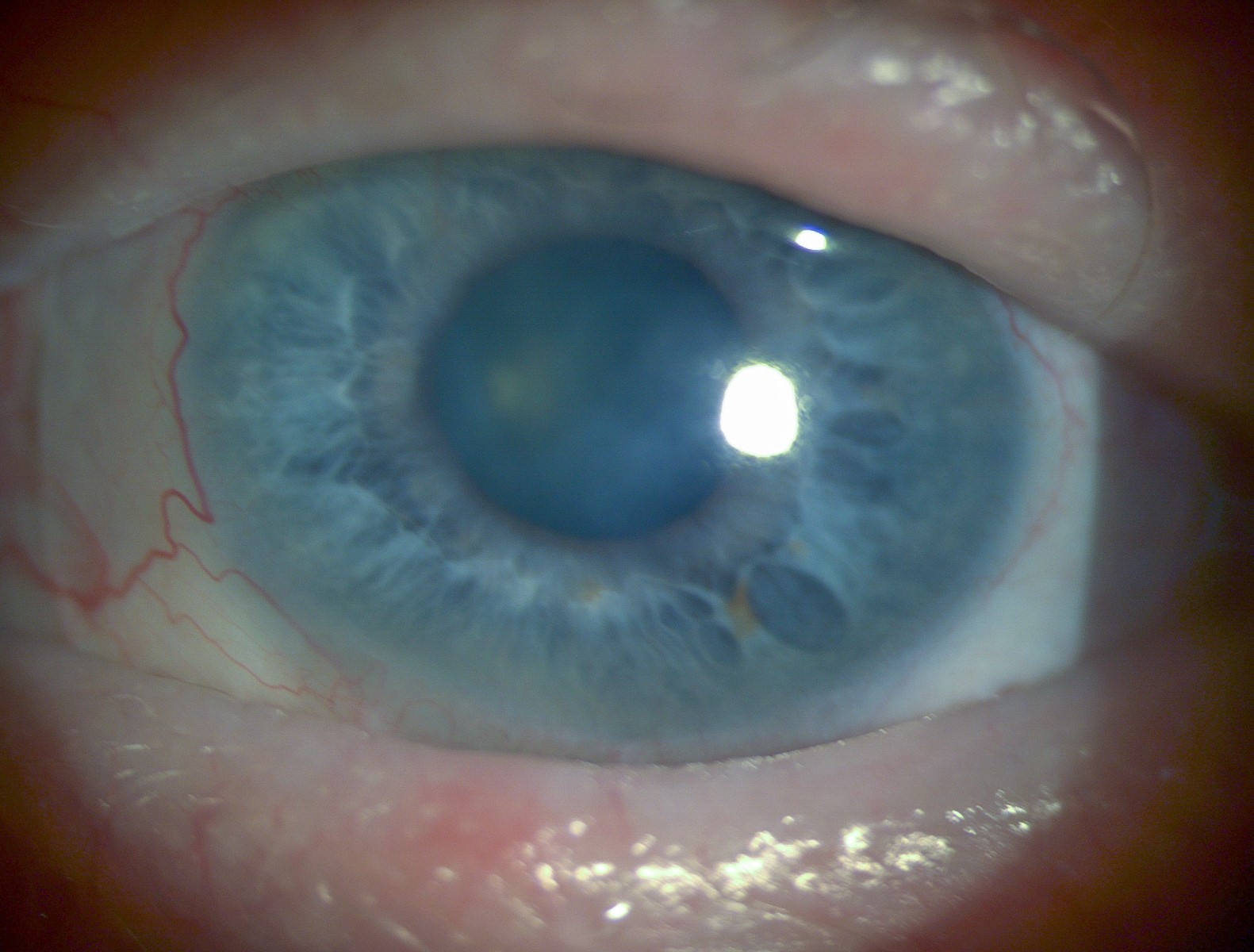
Figures 2a and 2b: View of anterior segment OD/OS: Sparse lashes of upper and lower eyelids, inflamed lid margins and bulbar conjunctiva, and subepithelial scarring of the central cornea with accompanied thinning.
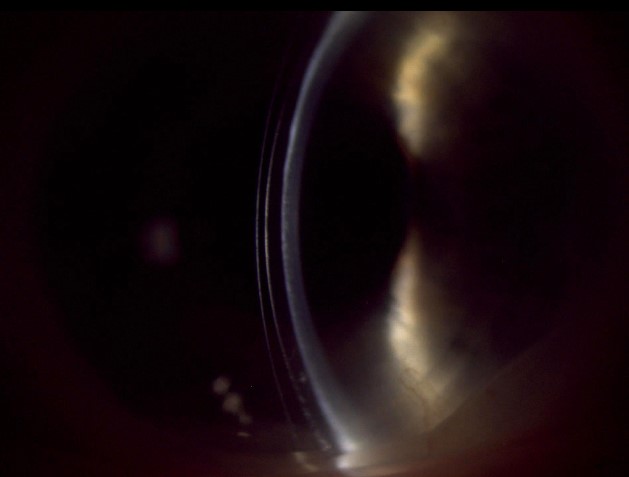

Figures 3a and 3b: Slit lamp view of scleral lenses OD/OS with optic section demonstrating adequate fluid reservoir clearance over areas of scarring and thinning.
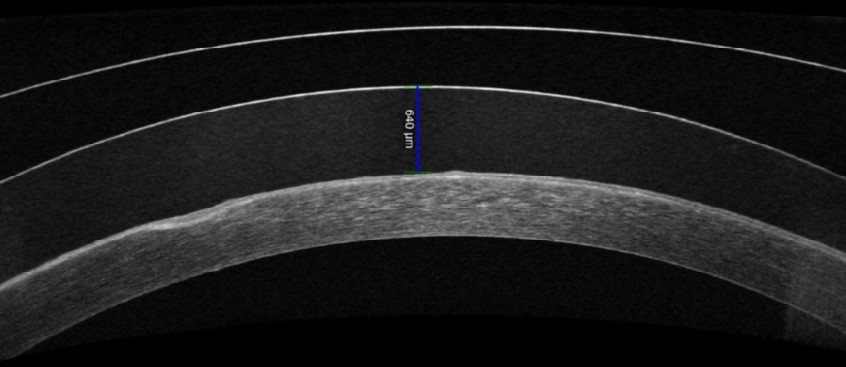
4a: 640 µm of clearance over area of scarring and irregularity.
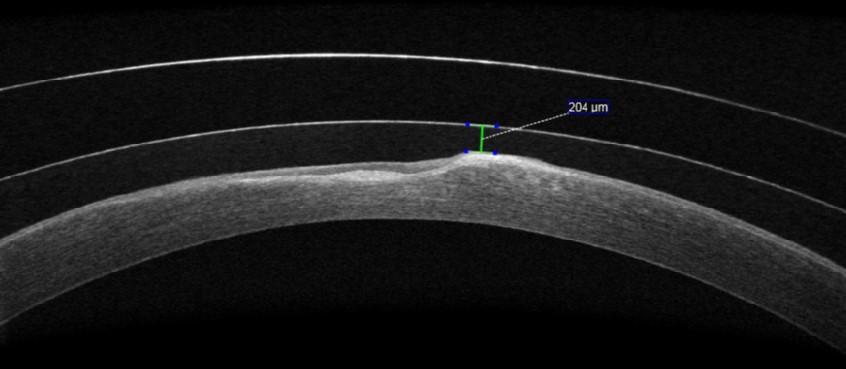
4b: 204 µm of clearance over area of scarring and irregularity.
Figures 4a and 4b: AS-OCT of final lens design.
Type | Power | BC | Diameter | Total Sag | Edges by Quadrant | Material | |
OD | FSE1 | -16.61 | 7.98 | 17.0 | 2455 | 1: +150 2: STD 3: +150 4: +150 | |
OS | FSE1 | -7.39 | 9.72 | 17.0 | 2300 | 1: STD 2: STD 3: STD 4: STD |
Table 1: Final scleral lens design OD and OS
Case 2:
56-year-old Caucasian male presented with eye irritation and blurred vision. H/o of EEC syndrome (ectrodactyly, ED, and orofacial clefts)
Ocular history of limbal stem cell deficiency, keratoconjunctivitis sicca and severe primary open angle glaucoma. Patient reported eye pain OD>OS while using habitual SLs. Impressions were obtained. Custom, impression-based SLs improved patient comfort and reduced ocular inflammation after 1 month of wear.
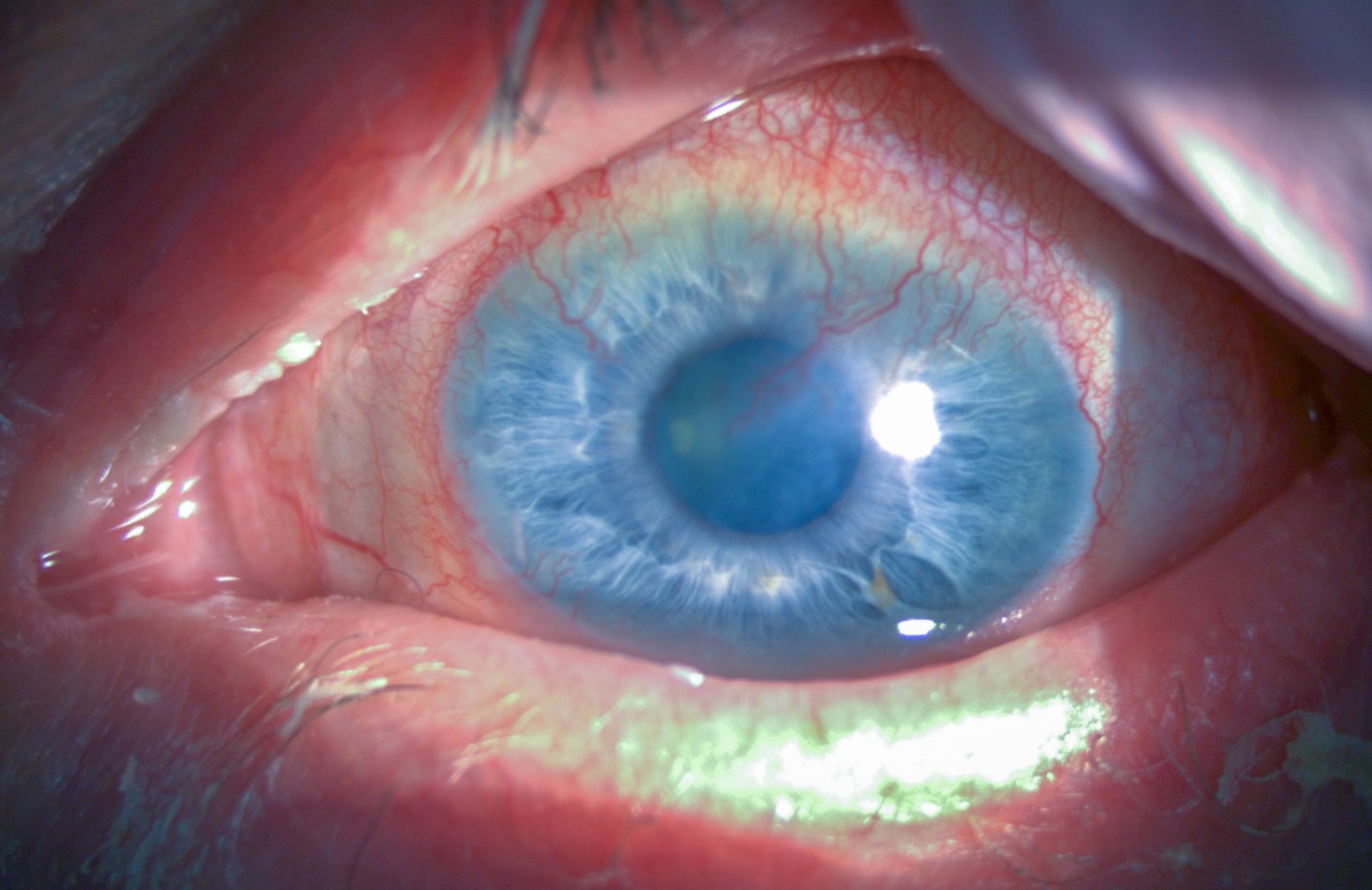
Figures 5a and 5b: Initial appearance OD/OS: Irregular/thickened lid margins with telangiectasia, diffuse conjunctival injection, and peripheral corneal stromal haze with neovascularization involving the visual axis.
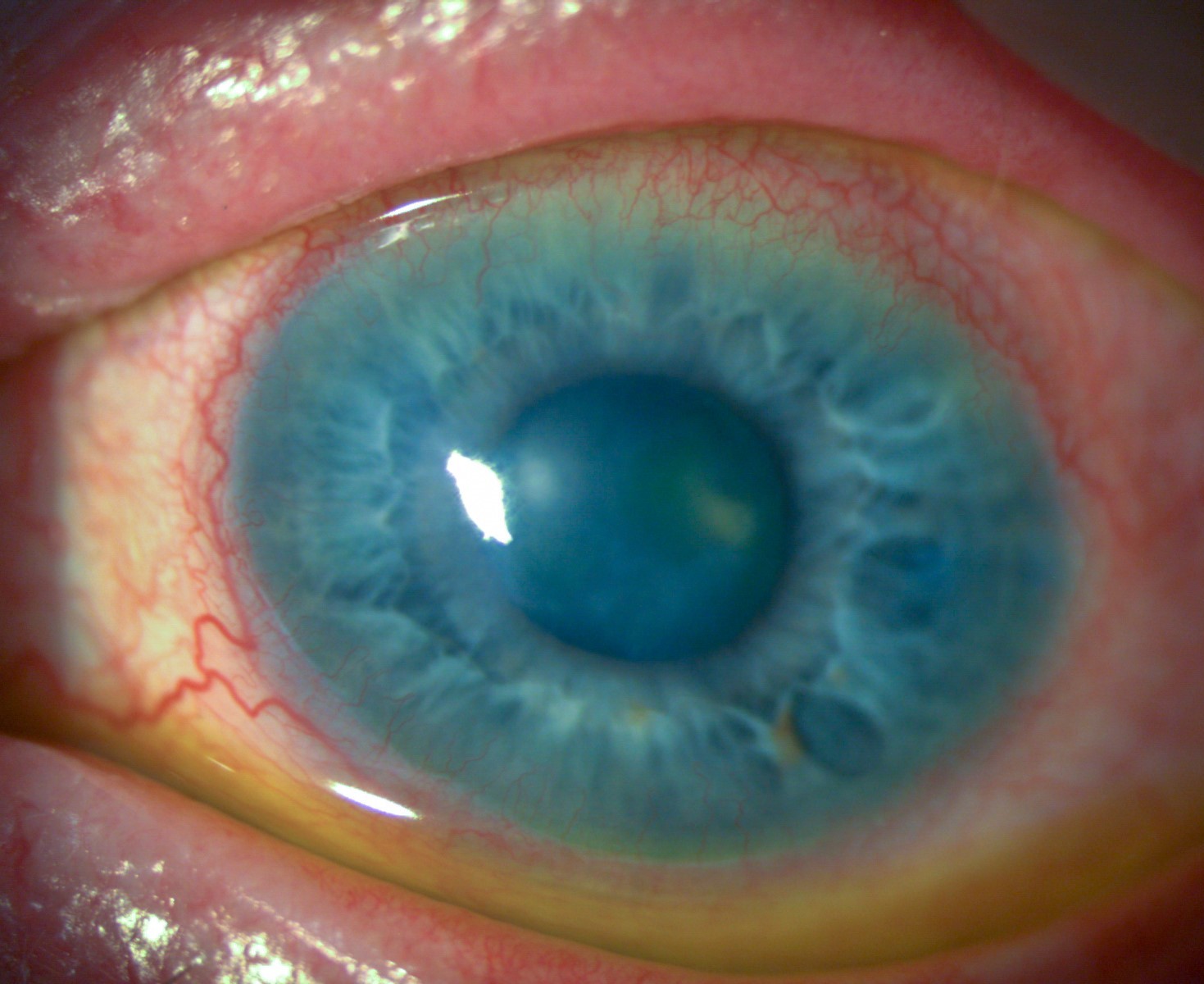
Figures 6a and 6b: View of OD/OS after 1-year of SL wear: Reduced ocular inflammation and regression of corneal neovascularization without surgical intervention.
Type | Power | BC | Diameter | Back Optic Zone Diameter | Material | |
OD | -3.75 | 8.058 | 16.5 | 9.24 x 7.85 | Optimum Extreme with HydraPEG | |
OS | -7.75 | 7.541 | 16.0 | 10.17 x 8.07 | Optimum Extreme with HydraPEG |
Table 2: Final scleral lens design OD and OS
Conclusions
This case series demonstrates the benefit of customized SL fitting with increased diameter to protect the cornea and conjunctiva of patients with ED. Improved SL fit and concomitant use of autologous serum can prevent further corneal scarring.
Both patients benefited from advanced SL customization which improved comfort and wear time. Scleral lenses effectively address multiple concurrent ocular issues, and achieving an accurate fit can significantly enhance long-term comfort, wear duration, and overall quality of life.