Introduction
Clinical Presentation
A 54-year-old female presented for a corneal evaluation due to decreased vision and severe right eye pain. She had a history of being treated for suspected Herpes Simplex Virus (HSV) and neurotropic keratitis 2-3 months prior to being seen at Havener Eye Institute without symptomatic relief. She also had a history of primary soft contact lens wear due to poor adaptation to vision in spectacles. She discontinued contact lens wear due to symptoms.
Chief Complaint: pain, blurry vision, tearing, burning, photophobia OD
Ocular History: corneal ulcer and scar OD
Ocular Surgeries: none
Ocular medication:
- Failed Therapies:
- Autologous Serum 6-8x per day OD
- Ofloxacin QID
- Prednisolone acetate 1% ophthalmic suspension BID
- Cyclosporine Ophthalmic Emulsion 0.05% BID OU
- Erythromycin ointment QPM OD
- Cenegermin-bkbj ophthalmic solution 0.002% 6x per day
- Valacyclovir 1g PO BID
- Amniotic membrane
| Entering Testing and Slit Lamp Findings | OD | OS |
| Entering Uncorrected VA | HM (PH: NI) | 20/150 (PH: 20/40) |
| Intraocular Pressure | 10mmHg | 9mmHg |
| External | Reactive ptosis | No Abnormalities |
| Lids/Lashes | No Abnormalities | No Abnormalities |
| Conjunctiva/Sclera | 2-3+ injection | White and Quiet |
| Cornea |
|
All layers clear |
| Anterior Chamber | Deep and Quiet | Deep and Quiet |
| Iris | Round and Reactive | Round and Reactive |
| Lens | Clear | Clear |
Table 1. Entrance Testing and Slit Lamp Examination

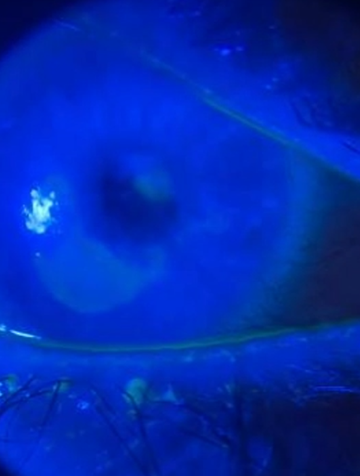
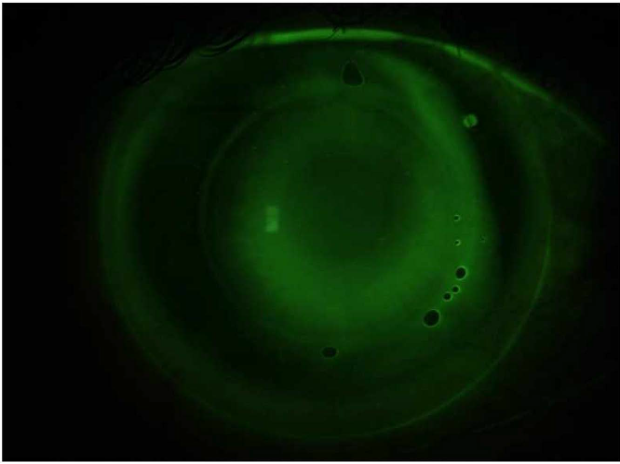
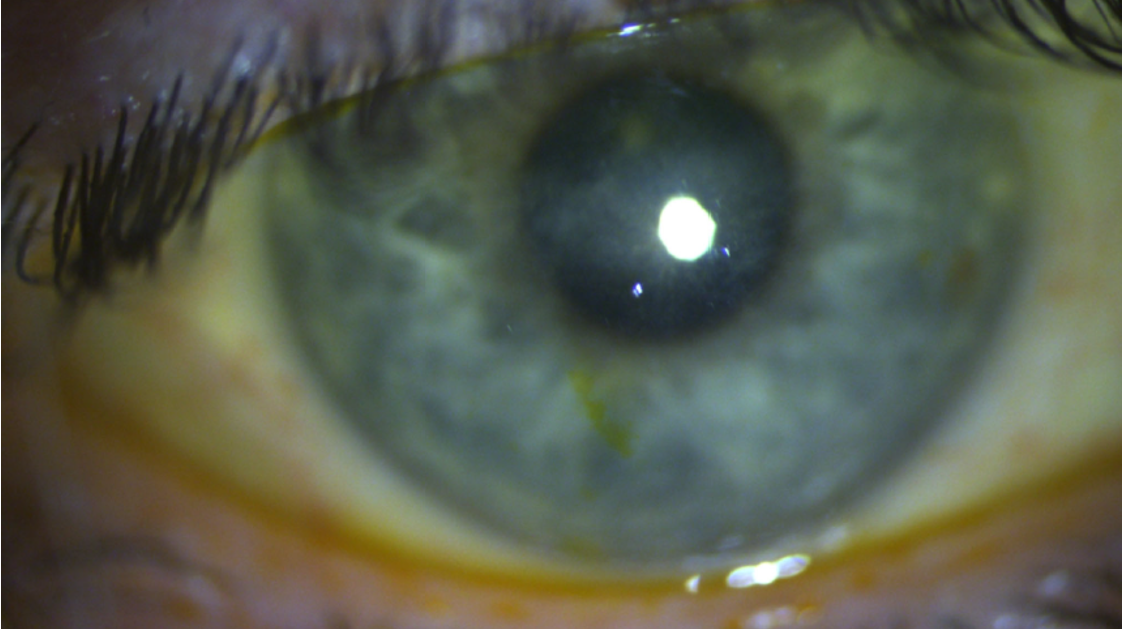
Figure 1 and 2. Slit lamp external photography of the patient’s right eye showing diffuse punctate epithelial erosions, a central circular anterior stromal scar with surrounding haze, and an overlying epithelial defect.
Methods and Results
Due to no improvement despite therapy, as well as a history of soft contact lens abuse and noncompliance, a corneal culture of the right eye was obtained. PCR results were positive for Acanthamoeba spp.
Treatment and Management
- Moxifloxacin TID OD
- Chlorhexidine QID OD
- PHMB Q1H OD
- Cyclopentolate BID
- Valacyclovir 1g PO BID
Contact Lens Fitting
OD: Upon resolution of active infection, the patient was referred by the corneal service for a scleral lens evaluation
OS: The patient was refit into a daily disposable soft contact lens
| Post Infectious Testing and Slit Lamp Findings | OD | OS |
| Entering VA w/ spectacles | CF at 3’ (PH: 20/200-1) | 20/25+2 |
| Intraocular Pressure | 10mmHg | 9mmHg |
| External | Reactive ptosis | No Abnormalities |
| Lids/Lashes | No Abnormalities | No Abnormalities |
| Conjunctiva/Sclera | White and Quiet | White and Quiet |
| Cornea |
| All layers clear |
| Anterior Chamber | Deep and Quiet | Deep and Quiet |
| Iris | Round and Reactive | Round and Reactive |
| Lens | Clear | Clear |
Table 2. Post Infectious Testing and Slit Lamp Examination
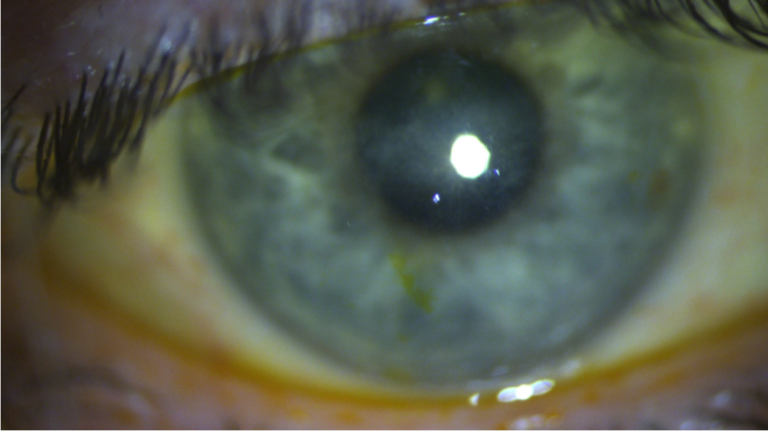
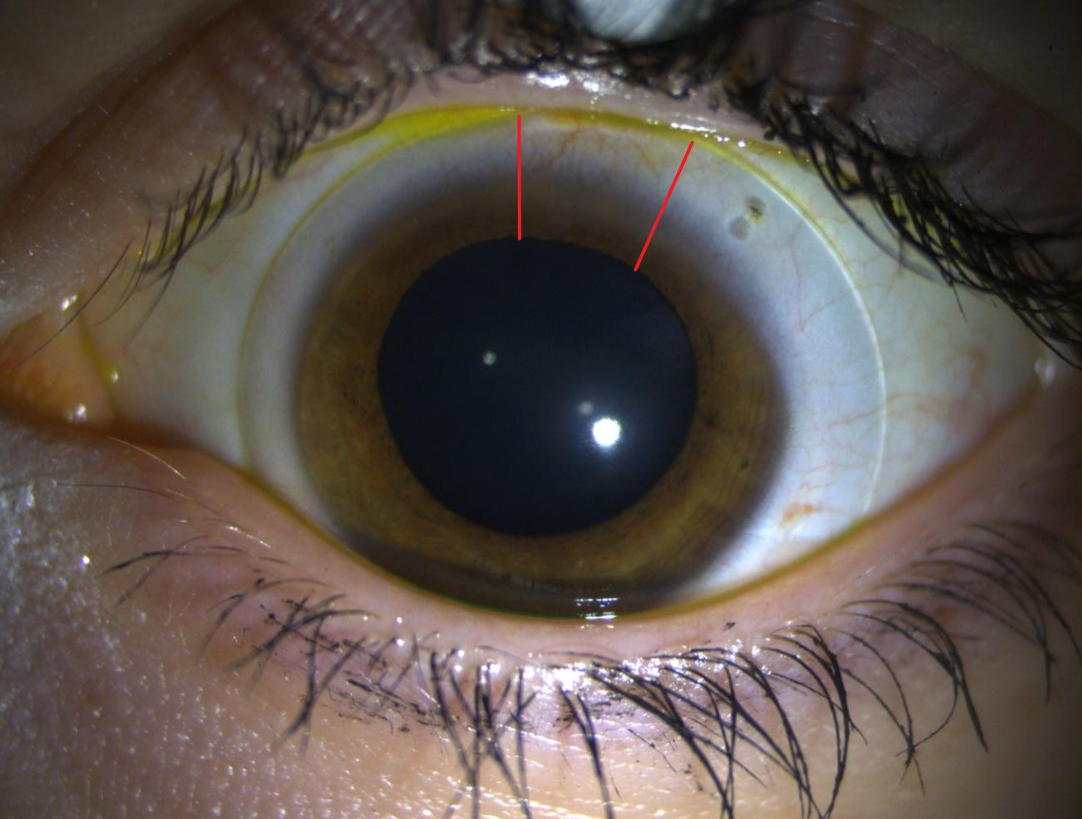
Figure 3. Slit lamp photography of, OD, central scar and stromal haze
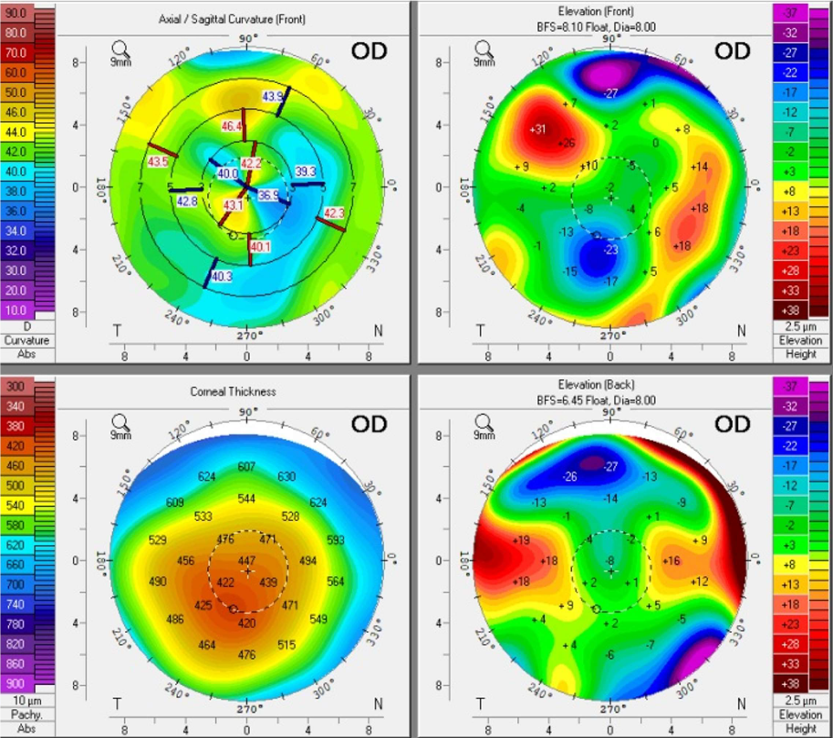
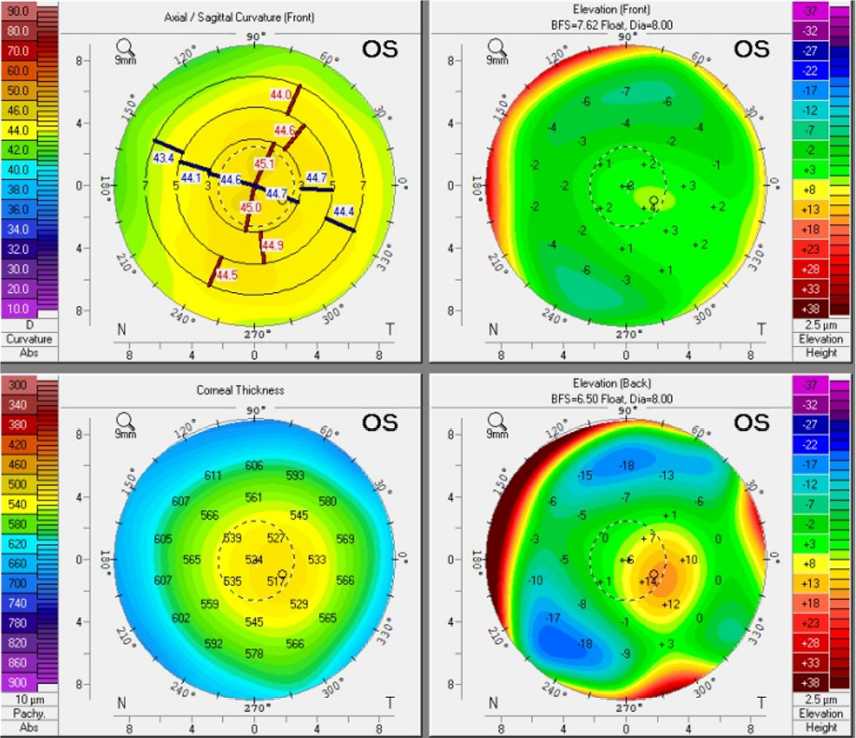
Figure 4. OD (right) and OS (left): Scheimpflug tomography
Clinical Outcome
OD
- BCVA: 20/40+2
- Mild irregular corneal epithelium overlying a central scar, faint neovascularization, and stromal haze
- No staining upon removal
OS
- BCVA: 20/20
- Well centered fit with adequate coverage and movement
- No staining upon removal
Final Lens Parameters |
|
|
|
|
|
|
Eye | Lens | Diameter (mm) | Base Curve (mm) | Power (D) | Material | Total Sag |
OD | BostonSight SCLERALTM | 18.0 | 8.0 | +0.75DS | 2750 | |
OS | Alcon Dailies Total 1TM | 14.1 | 8.5 | -2.75DS | Deleficon A | N/A |
Table 3. Final Lens Parameters
Discussion
Patients suffering from AK present with eye pain, lacrimation, redness, blurred vision, and foreign body sensation. AK usually presents unilaterally, with only 7.5% of cases presenting bilaterally1-2. Early clinical indicators of AK include an irregular epithelium and pseudodendrites, which can advance to radial keratoneuritis, as well as diffuse or focal anterior stromal ring infiltrates. In severe cases, AK may progress to conditions such as limbitis, scleritis, uveitis, and corneal melt, potentially resulting in perforation if untreated.
Diagnosis of AK can be challenging due to the variance in clinical signs and symptoms. HSV keratitis, fungal keratitis, and Pseudomonas keratitis are all important differential diagnosis to consider. However, early detection of AK is the most critical factor for achieving a favorable visual outcome due to the infection being limited to the superficial cornea. The average delay in diagnosis of AK is 50 days after the first presentation of symptoms. If the disease persists for more than 4 weeks without appropriate treatment, the final visual prognosis is less favorable with 25% of AK cases result in the need of a penetrating keratoplasty3-4.
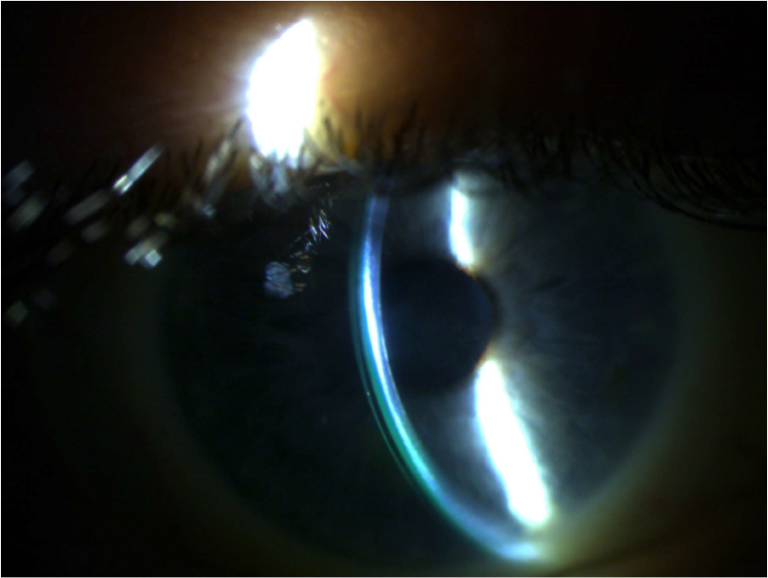
Figure 5. Slit lamp photography of, OD, final scleral lens with an optic section
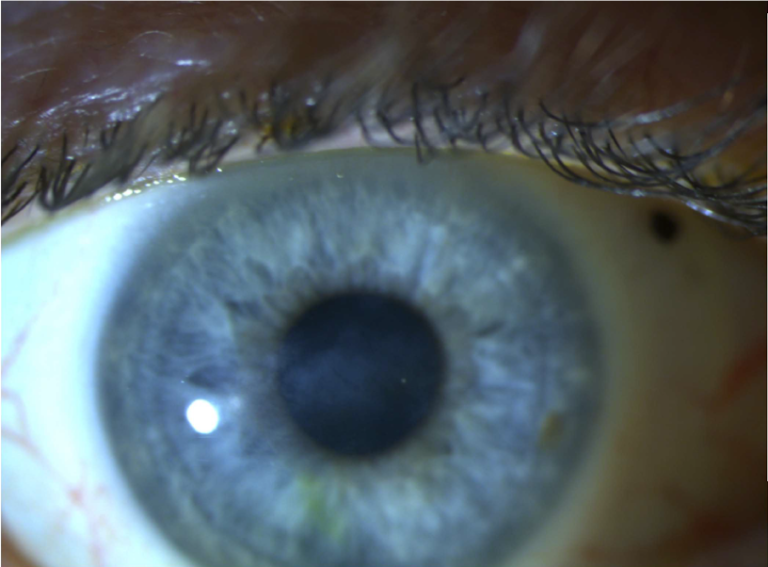
Figure 6. Slit lamp photography of, OD, final scleral lens in primary gaze
Conclusion
A high clinical suspicion of AK should be present in primary contact lens wearers with a history of noncompliance. Corneal culture or confocal microscopy are imperative in identifying corneal pathology when conventional treatment is ineffective. The current treatment approach for AK involves debridement of the infected epithelium as well as PHMB and Chlorhexidine with medical treatment lasting 3-6 months3-4. Scleral lenses are indicated after the active disease process has subsided to provide the best visual outcome over resulting corneal scars, sub epithelial haze, and irregular astigmatism. Educating and emphasizing proper contact lens hygiene is vitally important in insuring the corneal health of patients.