The “Contacts with Conway” series of YouTube videos have been surprisingly well-received by both industry and the public. So much so in fact, that we regularly receive requests to explain or expand upon particular topics and, where possible, we use this feedback when deciding future episodes.
One such request came in recently and initially surprised me. It requested instructions for cleaning and caring for gas permeable contact lenses. Initially, I thought what could possibly be simpler? I then realised that there have been some quite confusing messages sent out since the days of PMMA, when I would recommend that patients clean their lenses with washing-up liquid or baby shampoo*, and so maybe some clarification was required.
With the growth in the use of gas permeable lenses and the introduction of more complex polymers such as Optimum Infinite for sclerals and orthokeratology, there is clearly a gap in the knowledge base concerning their care and maintenance. These new modalities represent quite an investment on the part of both patient and practitioner, and so I thought I would take time to come up with a straightforward guide for both parties.
There are three steps required to ensure that gas permeable lenses remain safe and comfortable during wear.
- Cleaning
After wear, the lens can be coated with greasy deposits from the tears (lipids, mucin and proteins), as well as cosmetics, soilants from the wearer’s fingers (heaven knows where they’ve been!), and dead cells from the normal metabolic processes of the eye. - Disinfection
During storage, normally overnight, the lens should be kept free from bacteria and other pathogenic contamination from its environment (the case), and any bugs that were on the lens from failure to complete step 1 should be eliminated or reduced to a level that will not cause an issue. - Conditioning
This is a process that occurs during soaking. Whereas steps 1 and 2 are common to all lenses including PMMA and soft lenses, step 3 is not well understood by patients and practitioners alike. It occurs during soaking overnight. All gas permeable lenses need this conditioning process to occur to get the best performance from their lenses.
Cleaning
Cleaning is, in my opinion, the most important step in all reusable contact lens care, including GPs, so please excuse me if I labour this section of the article. It is also the step that patients are least likely to do properly or not at all. It might be that they are poorly instructed, frightened to damage the lens, or are just too relaxed about their eye health – or probably a combination of all three.
If a gas permeable lens is properly cleaned then all of the possible contaminants and pathogens that might cause discomfort or infection in later use can be removed, or reduced to an insignificant level.
It is a shame that successful wearing of the lens should pivot on the very step that the patient is least likely to perform. This is why its importance should be stressed at every follow-up visit.
It is probably for this reason that one of the larger solutions manufacturers seized the opportunity to capitalise on their competitors by claiming that their multipurpose solution was a “No Rub” product. A stroke of marketing genius: the product was an immediate success, and competitors rushed to make the same claim. Patients bought into it because they all knew that they weren’t following the instructions of their practitioners and here was a product that allowed them to safely avoid that step altogether. The claim was later withdrawn. Clinical studies¹ concluded that the Rub/Rinse step was essential, but that news never reached the patient population with the level of hype of the earlier claims.
In the early days of contact lenses, separate solutions were required for cleaning and storage and this worked well. Patients were given a cleaning product and this served to remind them that this step needed to be done.
The introduction of the multipurpose solution was another attempt to gain a market advantage by “simplifying” the care regimen and assuring compliance. What actually happened is that the patient read on the bottle that the product “ Cleans, Disinfects, and Conditions” their lenses. They assumed that the solution had some magical chemical property that would do all three steps without the need for that tiresome Rub/Rinse step and who could blame them?
Case Example
I think now would be a good time to introduce the case of a patient fitted with sclerals by my colleague, Mark Darling. The patient had keratoconus and had been successfully wearing sclerals for some time when he reported a problem with his left eye. Upon examination, the right lens appears fairly clean and the upper lid shows the start of Giant Papillary Conjunctivitis (GPC), but the left lens is heavily coated and the lid shows GPC Grade 4. After questioning, the patient disclosed that he habitually removed the right lens first and cleaned it thoroughly as instructed. He then removed the left, and could not see clearly! In order not to risk damaging the lens, he placed it directly into the storage case. His use of Progent had slipped to “now and again”.
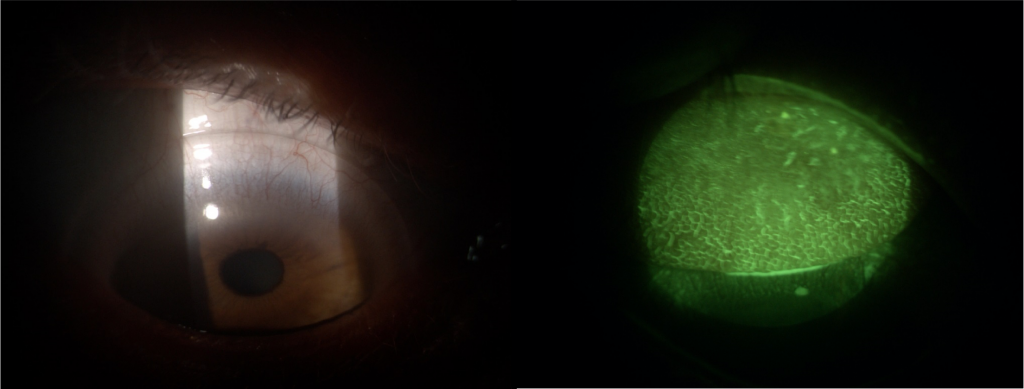
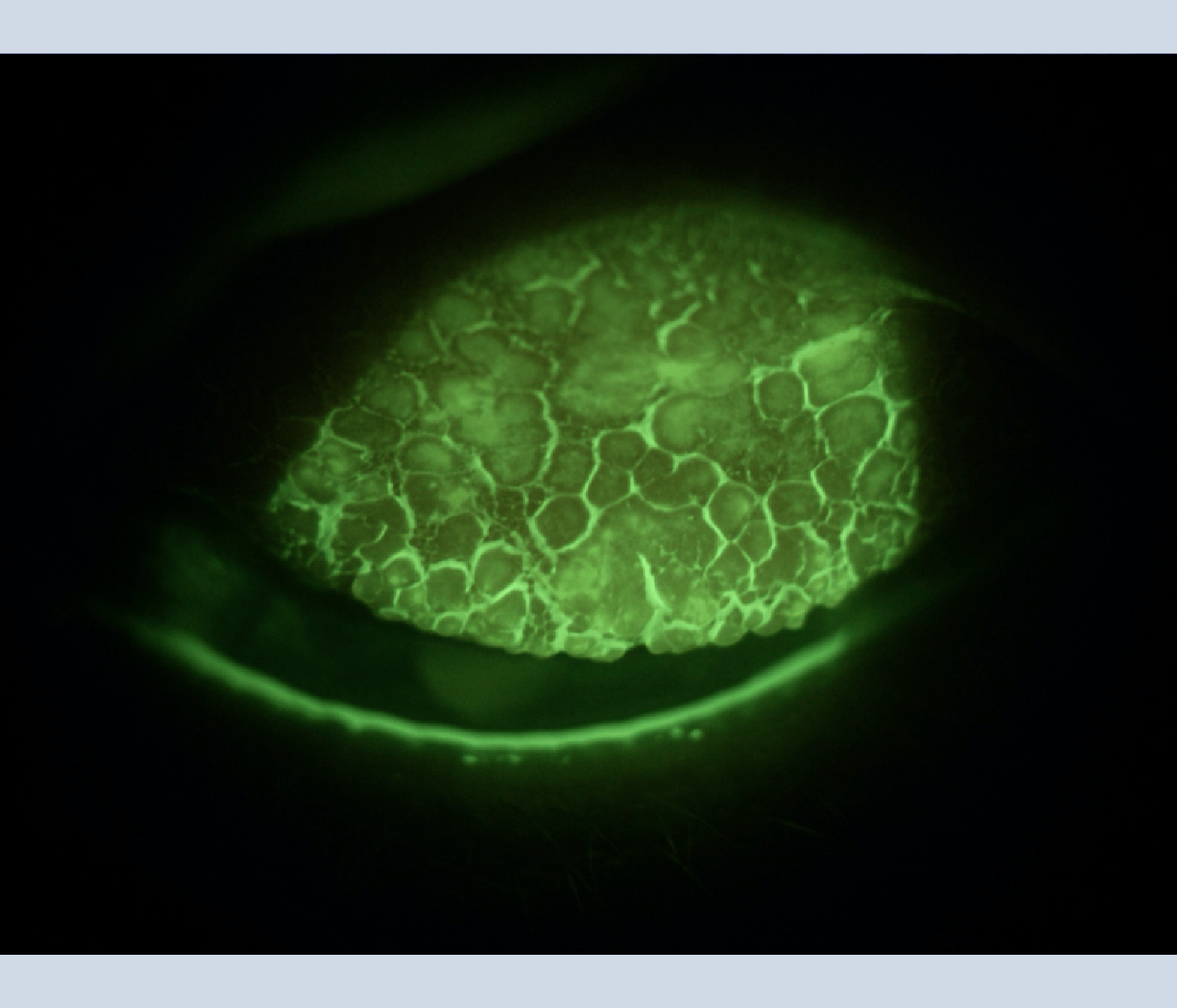
Fig 1 and 2. Right eye and right lid.
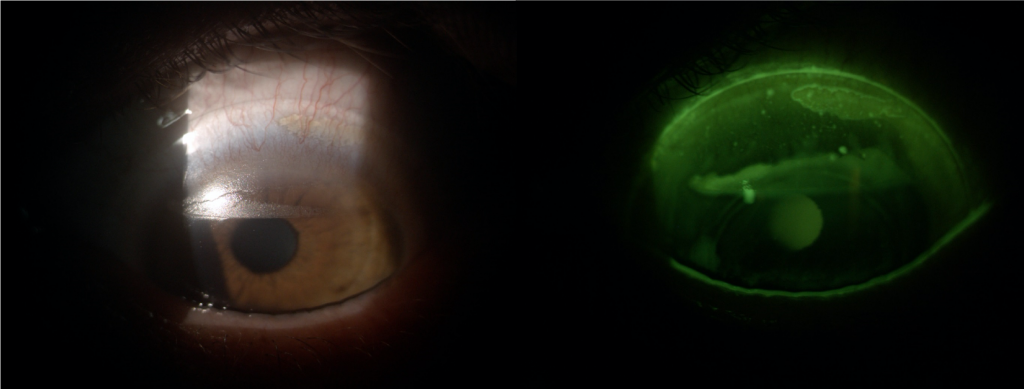
Fig 3 and 4. Left eye and left eye with fluorescein.
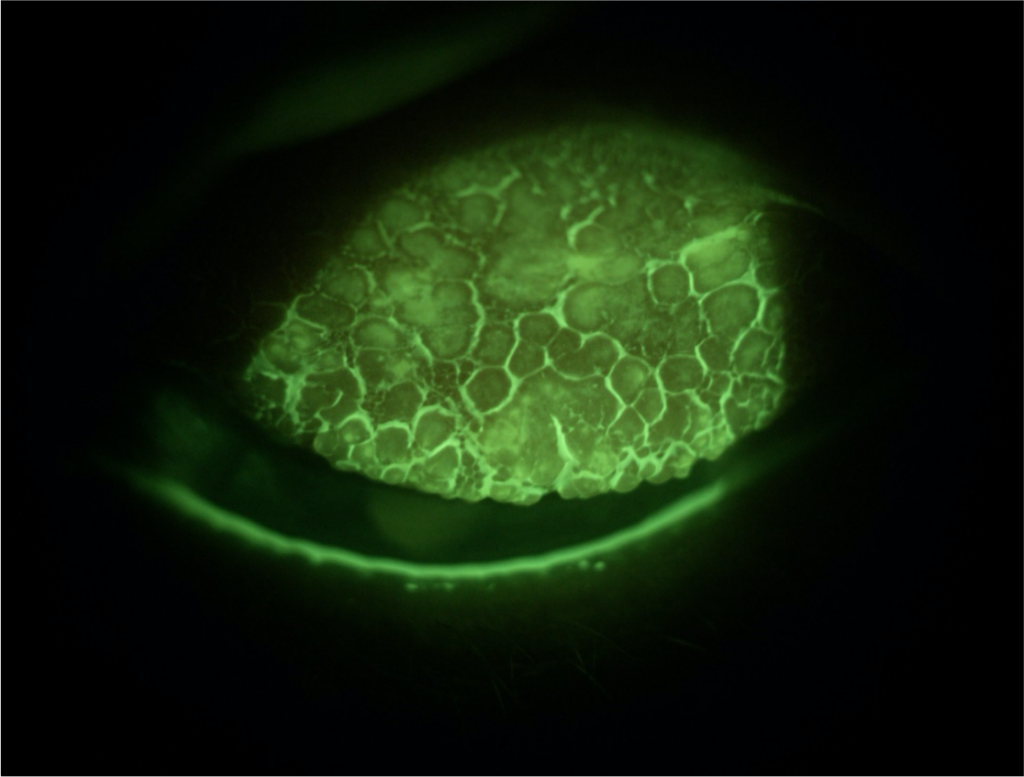
Fig 5. Left lid showing Grade 4 Giant Papillary Conjunctivitis.
This case clearly demonstrates the difference that the Rub/Rinse step can make to a patient’s welfare. The remedy for this patient? After treating the GPC, he now alternates between right and left lens for removal first, and Mark accepts that the lenses are now both receiving a balanced cleaning step albeit slightly less than ideal. By adding a weekly Progent treatment any residual deposits are hopefully removed and, so far, it appears to be working.
Solutions
I think it is worth noting that using a multipurpose solution does not necessarily mean that cleaning efficacy is compromised in any way provided that the patient does the Rub/Rinse step. Biotrue for example is my solution of choice for scleral users. It is an excellent surfactant and isn’t as viscous as some products, which makes rinsing prior to insertion easier. And yes, it is ok to use a soft lens product with GP lenses, but not the other way round I should add!
We are frequently asked by both laboratories and patients to recommend a cleaner for a given material/patient. Even though some newer materials have much more complex formulations than perhaps their forbears did, GP lenses are generally resilient and almost any surfactant may be used on the lens surface without fear of contamination or damage. The exception to this are lenses coated with the Tangible Hydra-PEG™ coating which can be disrupted if the wrong cleaner is used.
I suppose I should mention the use of peroxide with GP lenses. I am an advocate of peroxide generally, and it does offer some cleaning effect, but still not sufficient, in my opinion, for every patient. I know that manufacturers will suggest a Rub/Rinse step prior to soak, but patients don’t like doing it. The solution is too watery, and it makes their fingertips go white! For sclerals, the baskets are too small for most lenses and the risk of damaging an edge is increased. For patients who appear to be sensitive to other solutions, it is tempting to use peroxide, but you really need to introduce a separate cleaner first for most patients. GP materials have minimal uptake of solutions, so little is absorbed by the lens, and a saline rinse should remove any residual solution that the patient imagines is affecting them. A separate insertion solution is required even for corneal GPs and so a simple disc-neutralised peroxide system is generally not sufficient on its own.
Disinfection
The disinfection step is designed to kill or significantly reduce a specific range of pathogens associated with eye infections. During testing, an inoculum of standard pathogens is introduced into the solution and the solutions need to kill or reduce the quantity of those to pre-specified levels over a given time frame – all well and good.
This process does not involve a lens, however. In the real world, with a soiled lens, the biofilm that builds up during wear on the surface of the lens protects any underlying bacteria or fungi from the disinfectants thus reducing the efficacy of the solution.
So we see that the cleaning step not only removes debris, reducing the pathogenic burden on the lens but removes the protective biofilm, exposing any surviving pathogens to the disinfectant. This means that the disinfectants in the solution can be at a much-reduced concentration and thus reduce the potential for ocular irritation.
This is where it can all go horribly wrong. Without going into detail on the various brands available, I wanted to once again emphasise the importance of the Rub/Rinse step as the most important step in the care of lenses.
Conditioning
Having briefly covered disinfection and banged on about cleaning ad nauseum, I think it’s worth talking about conditioning. This requirement is peculiar to GP lenses as all GP materials contain both hydrophobic and hydrophilic elements. The surface of the lens needs to be changed at a molecular level to bring the hydrophilic elements of the material to the surface and push the hydrophobic elements away from the surface to ensure that the surface remains wettable and comfortable. This process is what we refer to as conditioning. This needs to be done overnight during soaking and is reversible in both directions. It is the reason why lenses should arrive from the laboratory in solution, to allow this process to take place before the patient first receives them.
During wear, lipids collect on the surface of the lens and these are hydrophobic. They repel the hydrophilic elements that were present at the surface of the material and attract hydrophobic elements to the surface, leading to dry areas forming on the lens under the lipid.
During overnight soaking, the wetting agents present in the soaking solution reverses this process by repelling the hydrophobic elements and attracting the hydrophilic elements back to the surface to return the lens to optimal wettability.
Once again, failure to remove any lipid contaminants that collect on the surface of the lens can seriously compromise this process by masking the dry areas from the effect of the solution.
To demonstrate this effect, I left a scleral lens overnight in solution, but with a small spot of grease on the surface. In the morning the grease was still there and was easily removed with a surfactant, so the lens surface looked clear on visual inspection. I then wore the lens whilst a colleague filmed the surface. The dry spot corresponding to where the grease used to be was clearly visible, showing that the surface chemistry had been changed due to contact with the grease. The remedy? Remove the grease with a Rub/Rinse surfactant and a soak in solution to “recondition” the surface back to wettability.
So here again, this vital step in GP lens care is adversely affected by failure to completely remove a contaminant from the surface.
Conclusion
I guess by now you may have realised that, in my opinion, at the heart of safe GP contact lens care is effective cleaning and that there is no substitute yet for the very basic Rub/Rinse step. There have been accessories such as cleaning sponges and ultrasonic devices, but none are as effective as a digital clean. There are some patients with rough hands or such poor vision that they simply cannot or will not comply with this step, and a peroxide system can definitely be beneficial in such cases.
I have hesitated to mention specific brands in this article, but there is one product that I feel I must make an exception for, and that is Progent from Menicon. By introducing this catch-all treatment for RGP wearers that show a build-up of debris on an occasional basis, you can avert the situation that I described above. The frequency of use does not necessarily have to be weekly, but maybe bi-weekly or monthly depending on need. The one caveat I would offer is that Progent should not be used on a Tangible Hydra-PEG™ coated lens as it will totally strip the coating.
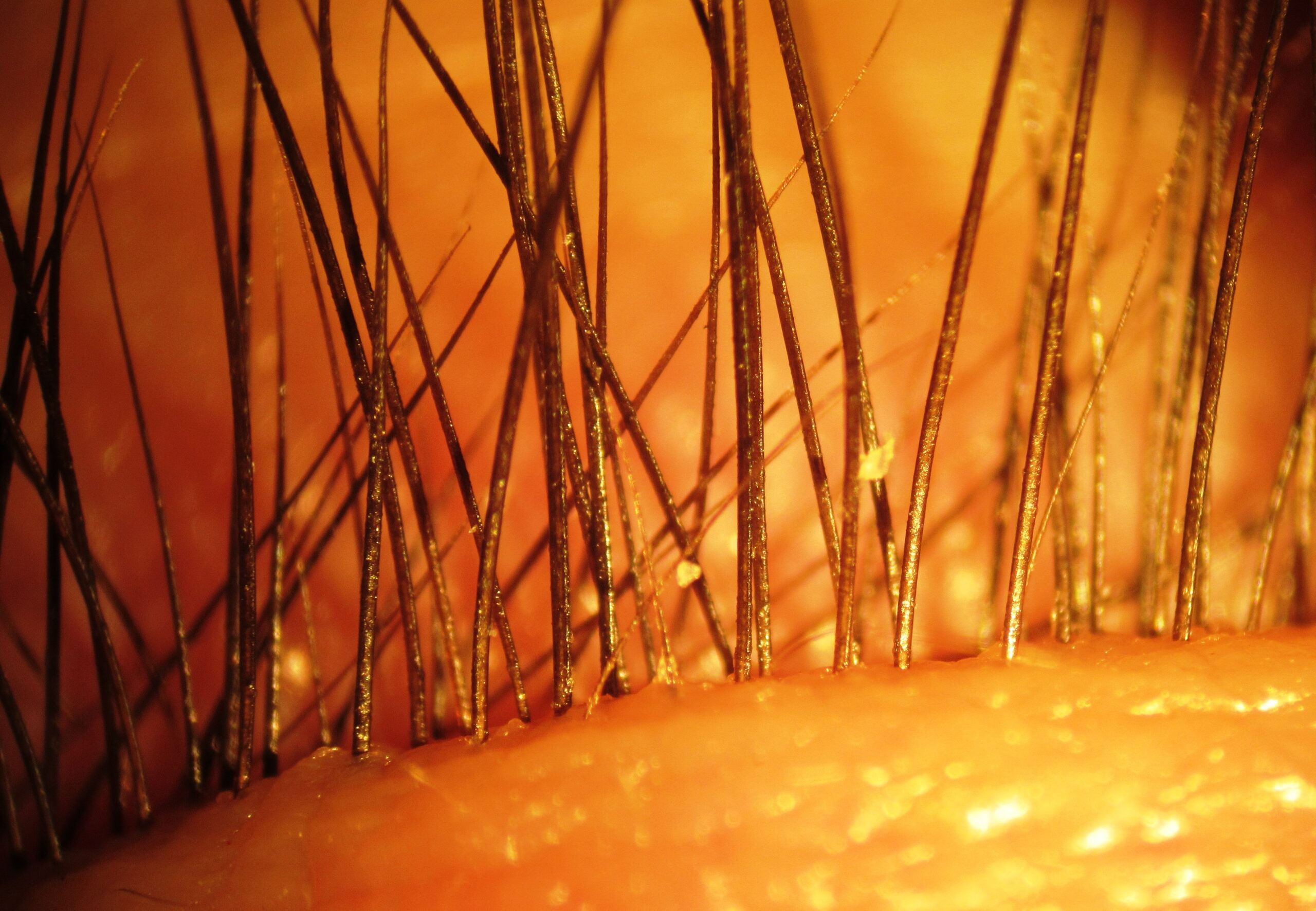
Finally, I’d like to sign off with an image supplied by a practitioner which demonstrates the sad fact that all of our scientific prowess and professional expertise means nothing when lenses are in the hands of unhygienic patients.

Stay safe and thank you for all the feedback and suggestions for “Contacts with Conway” – keep them coming.
*Washing up liquid and baby shampoo are not recommended for use in contact lens cleaning. Please follow your practitioner’s instructions for contact lens cleaning solutions.