Patient History
A 34-year-old Hispanic female was referred to us by an ophthalmology clinic for a contact lens evaluation. JS was diagnosed with keratoconus when she was 22 years old and claims that the vision worsened each year. She tried multiple pairs of glasses, and then she was finally fit with a corneal gas permeable contact lens. The corneal gas permeable lens provided good vision, but the discomfort prevented her from wearing it. She then proceeded to have corneal cross linking in each eye in early 2020.
When she saw us for an evaluation, we obtained an in-depth case history. JS told us that she was an LPN (Licensed Practical Nurse) for another doctor in town. Her duties included obtaining case histories from patients, performing tests such as blood pressure, taking temperatures, among others. She also administered injections. JS claimed that she was using the computer for 6+ hours per day. She stated that her very poor vision made it difficult to read the computer or exam notes. As a result, she constantly had to have other people read things for her because she mixed up letters and numbers frequently. Further, she complained of blurred vision, fluctuating vision, double vision, haloes around lights, and eye strain.
Patient Consultation
During her consultation, we performed several tests. The first test was a topography of each eye. The topographical maps provided valuable data so that we could get an idea of how steep and flat her eyes were, along with the overall shape of the cone, the elevation of different parts of her corneas, and her horizontal visible iris diameter (HVID). This information served as a baseline, and more topographies will be taken throughout the course of managing her case over the years.
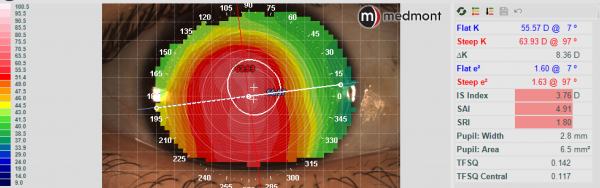
Topography – OD
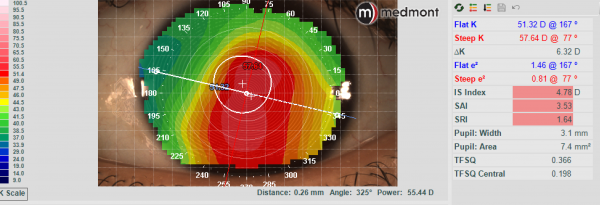
Topography – OS
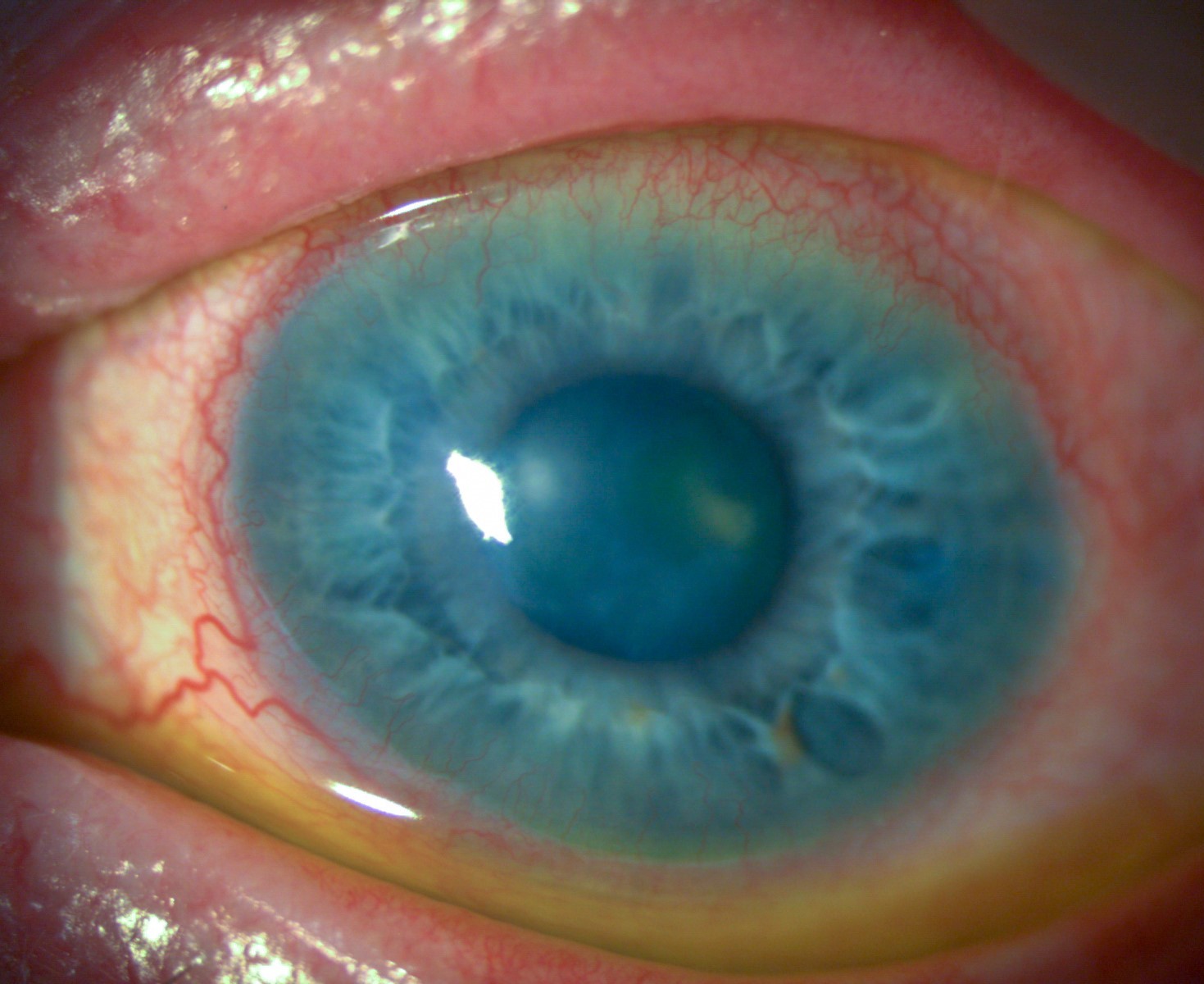
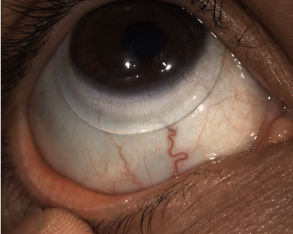
The next test was anterior segment photography. These photos provide a documentation of what the ocular structures look like at the time of the fitting. If any scarring, striae or other disorders are seen, photos are taken. This also serves as a good baseline so that if there are any changes in the future, we have something to compare it to.
We then performed a digital retinal wellness scan. This scan checks the macula and optic nerve to ensure there are no retinal abnormalities. This is not totally necessary when fitting a specialty contact lens, but I find it incredibly useful. Many times, if a patient is referred for a contact lens evaluation due to a corneal defect, they end up also having a retinal issue. This is important to discuss with the patient, as their vision potential could be severely limited when they have other ocular abnormalities.
Next, we performed a corneo‐scleral topography. This instrument checks the shape of the sclera. This data is incredibly valuable, as it can tell you the toricity of the sclera and the location of the toricity and elevation. This data helps us select an appropriate scleral lens for a patient. If a patient has a very highly irregular sclera, they may not be a good candidate for a traditional scleral lens. Also, if a patient has a more spherical scleral shape, you may consider a scleral lens that does not have toric haptics.
After all of the data is collected, a slit lamp examination is performed. After, a subjective refraction is attempted to find out the best corrected visual acuity in spectacles.
JS had entering visual acuities of 20/400 in the right eye and 20/400 in the left eye. With a subjective refraction, her vision did not improve in either eye.
Scleral Lens Fit
After reviewing all of her information, we discussed different contact lens options in depth, including corneal gas permeable lenses, hybrid lenses, and scleral lenses. After discussing the pros and cons of each lens, she opted for the scleral lens. Due to finances, she decided to proceed with fitting the right eye only at this time.
Her scleral lens shape showed about 150um of scleral toricity, which is why the Ampleye scleral lens was selected.
The diagnostic lens showed central touch so it was removed and replaced.
The next trial lens showed excessive central clearance, good limbal clearance, and good edge alignment. With an over‐refraction of +9.25, she was able to achieve 20/30 vision!
The final lens was ordered through Art Optical with a decrease in sagittal depth and incorporating the over‐refraction.
| BC | Sag | Power | OAD | Toric Haptic | |
| Diagnostic Lens | 8.04 | 4400 | -4.00 | 16.5 | 150um |
| Trial Lens | 8.04 | 4800 | ‐8.00 | 16.5 | 150um |
| Final Lens | 8.04 | 4600 | +2.25 | 16.5 | 150um |
Lens Material: Optimum Extra
Tint: Clear
Lens Dispense
JS arrived for her lens dispense and we inserted her Ampleye scleral lens in the right eye and she could achieve 20/30 vision immediately. She was thrilled with how well she could see. Central clearance was about 500 um upon insertion. The limbal clearance was adequate and the edges were aligned.
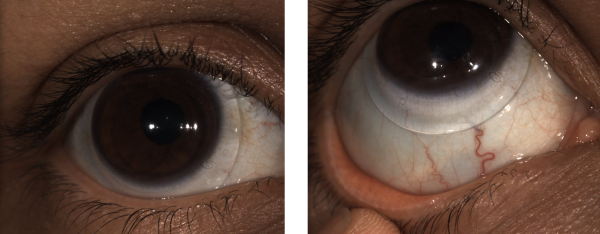
Scleral Lens – Central and Inferior – OD
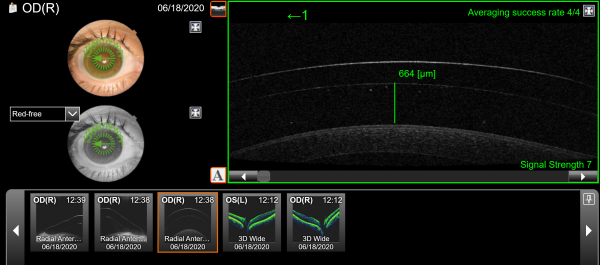
OCT – Scleral Clearance
We then completed an in-depth training, reviewing lens care and handling techniques. Several devices were used to demonstrate insertion techniques. She was shown 2 different lens care systems to properly clean, disinfect, and store her scleral lens. For scleral lens filling solution, Nutrifill was selected. Nutrifill contains electrolytes – sodium, phosphate, potassium, calcium, and magnesium – to mimic the body’s natural tears and support the ocular surface during prolonged lens wear.

1 day follow up
I called JS the next day to find out how she was doing with her scleral lens. She claimed that everything was in high definition! With her scleral lenses, she stated that she was able to see her computer at work clearly, and she was able to see a menu at a restaurant. She was thrilled with her vision and the comfort of her lens.
3 day follow up
JS called the office complaining that her vision was blurry with the contact lens in. She also stated it was not comfortable. I explained that there was likely an insertion bubble, and she should remove, refill, and reinsert the contact lens. She did as instructed, and was able to see clearly again. Insertion bubbles are one of the most common issues that arise with new scleral lens wearers. It is important to educate them on what to expect when they have a bubble (poor vision, lens discomfort, eye redness, irritation, and foreign body sensation). It is also important that they are instructed to remove the scleral lens, refill and reinsert. Many patients think the bubble will dissipate on its own, and this is not the case. The lens needs to be completely removed from the eye, and the patient should start over.
She will be coming in for her 3 week follow up very soon, and then we will be fitting her left eye into a scleral lens.
Conclusion
Scleral lenses are a viable option for patients with corneal irregularities, such as keratoconus. The gas permeable optics create a smooth surface for refracting light, which results in overall improved visual quality. Keratoconus patients can benefit highly from a gas permeable lens modality and should be considered as a treatment option to improve the vision.
Thank you to Dr Stephanie Woo, O.D. for contributing to Global Insight.