Background
Post-surgical ectasia is a complication in which a cornea that has undergone a refractive surgical procedure becomes progressively irregular and thinned leading to protrusion and undesirable visual disturbances such as blur and higher order aberrations. When screening a candidate for LASIK, many factors must be considered to reduce the risk of post-surgical ectasia; age, refractive error before surgery, topography before surgery, corneal thickness, and residual stromal bed.
Case Presentation
A 10-year-old middle eastern female is referred by her Primary Care Physician for decreased vision. She reported a mild decrease in vision over the last few years and was bothered by blur and shadowing.
POH: S/p LASIK at 3 years old, strabismus surgery at 4 years old
PMH: unremarkable
Medications: no medications
PFH: (+) postsurgical ectasia – father
BCVA w/ spectacles: 20/25+2 OD; 20/25-2 OS*
Preliminary Testing: normal EOMs; PERRL (-) APD; FTFC OU; CT ortho at distance and near
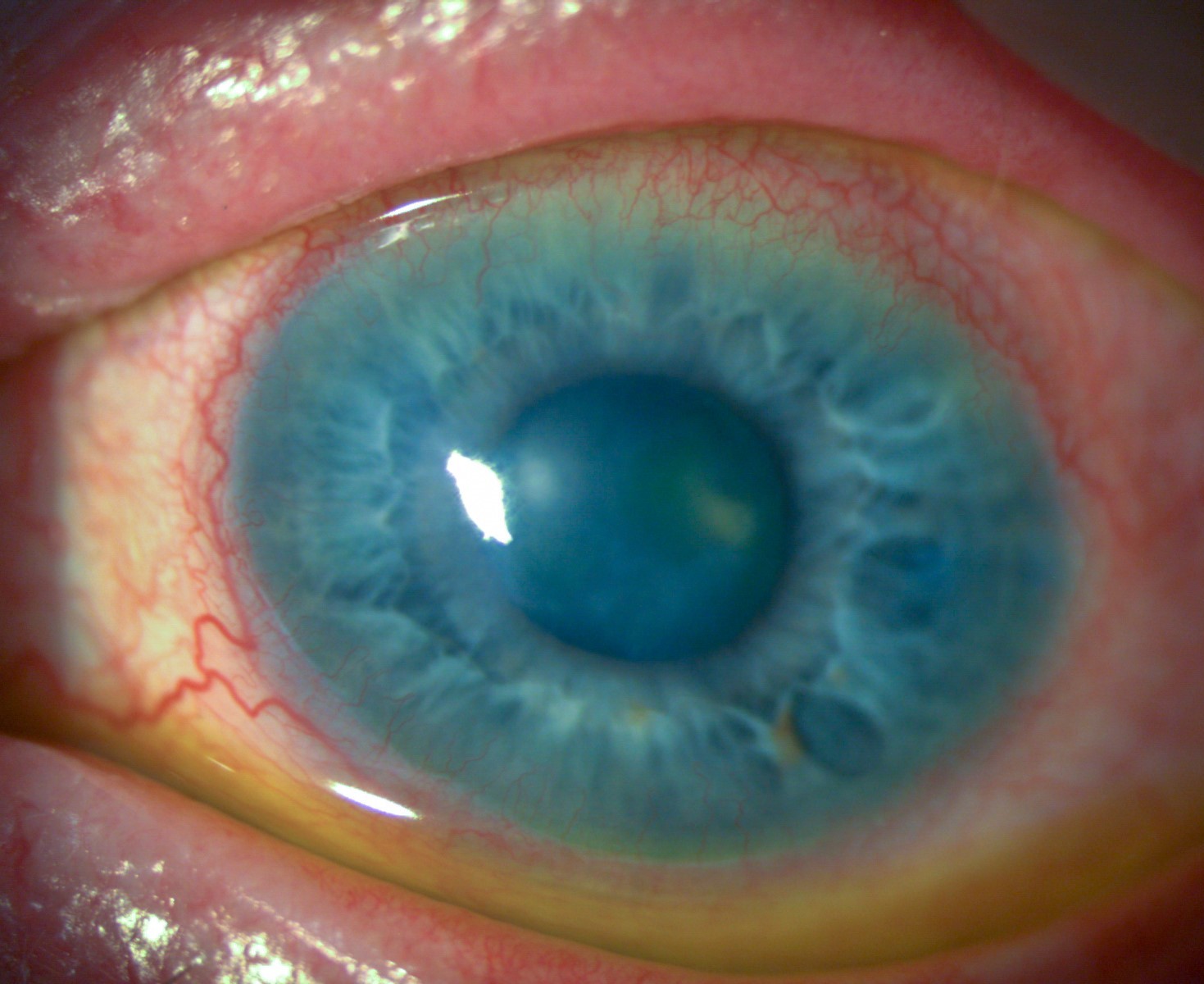
Slit Lamp Evaluation: LASIK flaps in place; (-) haze, (-) scarring OU
Ancillary Testing:
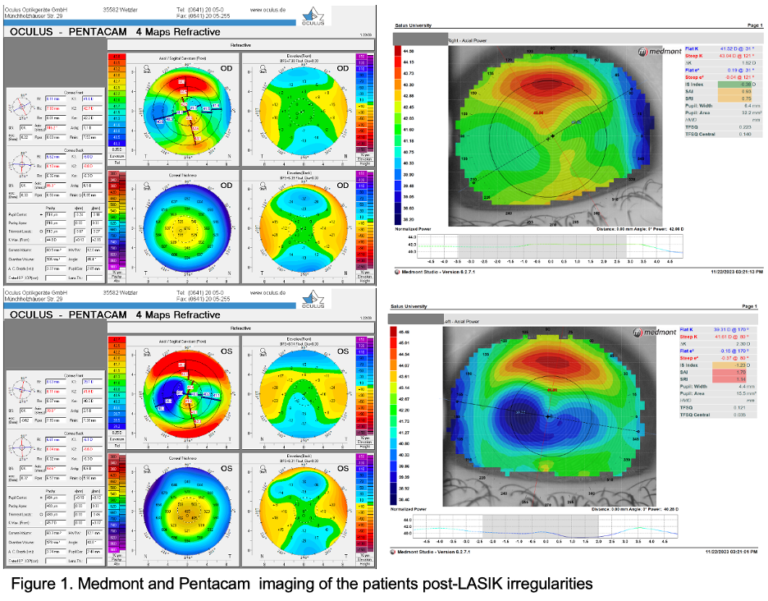
Topography: (OD) Flat K 41.6D; Steep K 42.7D; HVID 12.0mm, (OS) Flat K 39.1D; Steep K 41.6D; HVID 12.1mm
Pachymetry: (OD) 513um; (OS) 483um
Based on this presentation, all differentials for these corneal irregularities must be considered, such as keratoconus, Terrien’s marginal degeneration, and pellucid marginal degeneration. However, given this patient’s history and age, it is appropriate to conclude that her corneal irregularities resulted from the procedure she underwent at a young age.
* It is important to note that while vision is not measured to be remarkably reduced, irregularities on the cornea can produce higher order aberrations leading to decreased functionality of seemingly good vision, and given the age of the patient, the risk of progression is increased.
Lens Fitting
Corneal gas permeable lenses were chosen to provide superior optics while also being a lower cost option and having simple insertion and removal technique. A topography scan provided further information on the best starting point for fitting these customized corneal gas permeable lenses. A large diameter corneal gas permeable lens was chosen for both eyes with the addition of reverse geometry technology for the left eye.
When approaching a complicated fit as this case is, it is helpful to use all the tools available. At this teaching clinic, lenses from our fit set were placed on the eye at the initial visit to diagnostically determine which parameters needed to be changed. The first set of lenses ordered were designed based on the diagnostic fitting as well as the utilization of lens design software to better determine the degree of changes to be made.
Fitting Set:
(OD) BC: 8.04 || PWR:-0.62 || DIA:10.8 || EL: Standard
Fit: mild central bearing, patient reported discomfort
OR: -0.25sph
VA: 20/20-2
Plan: steepen lens and incorporate over refraction
(OS) BC: 8.65 || PWR:-0.37 || DIA:10.8 || EL: Standard Series C
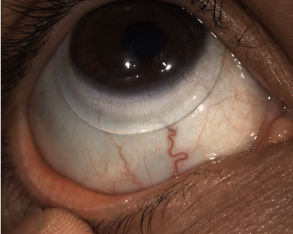
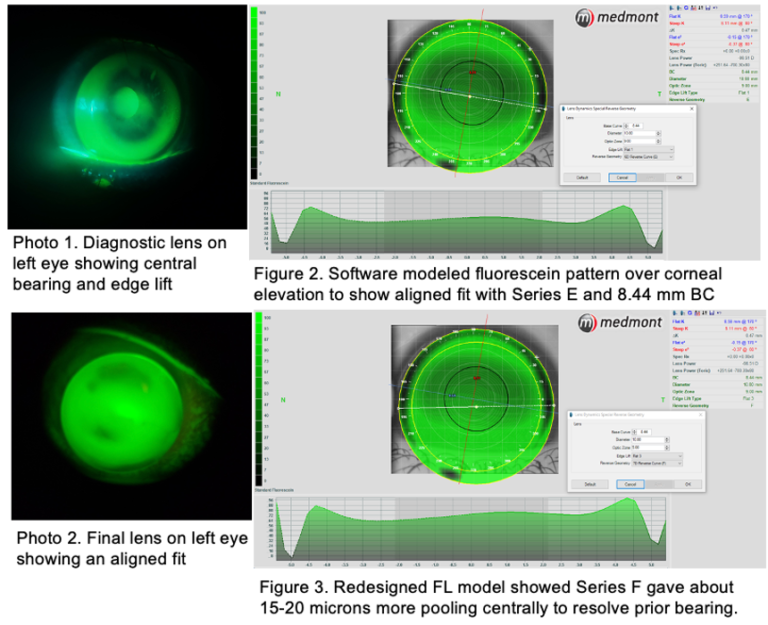
Fit: too much edge lift, bearing centrally (Photo 1)
OR: +0.25
VA: 20/25-3
Plan: increase reverse geometry and steepen BC
Follow-up:
(OD) BC: 7.89 || PWR:-1.62 || DIA:10.8 || EL: Standard
Fit: good fit with adequate tear exchange and appropriate comfort.
VA: 20/20
OR: plano
Plan: no changes
(OS) BC: 8.44 || PWR:-1.12 || DIA:10.8 || EL:1 Flat || SERIES E
Fit: central bearing, thin edges
VA: 20/20-3
OR: -0.25sph
Plan: increase reverse geometry, flatten edges (Figure 2)
Final Dispense:
Intralimbal GP- Optimum Extra Green
(OD) BC:7.89 || PWR: -1.62 || DIA:10.8 || ET:0.14 || EL:Standard || 1 DOT
VA: 20/20
Reverse Geometry GP- Optimum Extra Blue
(OS) BC: 8.44 || PWR: -1.37 || DIA:10.8 || EL:3 Flat || SERIES F
VA: 20/20-1
Conclusion
When screening candidates for the LASIK procedure, it is important to consider the age, refractive error before surgery, topographic pattern before surgery, central corneal thickness, and residual stromal bed. All these factors pose a risk for post-surgical corneal ectasia. The age at which this patient received the LASIK procedure puts her at increased risk for not only corneal ectasia, but further changes in her refractive error alone. There are few studies published that have explored the long-term stability of LASIK in children this young.
When fitting a custom specialty lens, it is important to consider the individual needs of the patient. This patient is at a visually demanding time of her life where decreased quality of vision may impact her education and other activities. This case demonstrates a successful fit of corneal gas permeable lenses that met the visual needs of the patient and relieved the shadowing and blur she reported at presentation. Patients with post-surgical irregularities should be closely monitored for further progression with repeat tomography. If further corneal changes are noted, the patient should be considered for corneal cross linking to halt the progression of postsurgical ectasia.